From an international driver to the client-centred care model; in this article Anthony Hogan explores outcome measures for individual goal setting and measuring those outcomes.
Introduction
When people present for hearing help, they are typically looking for solutions to the problems that they, or those around them, experience. These problems are inherently social in nature. Let’s face it – very few people will arrive at their first audiological consultation stating that they want help with their high frequency, sensorineural, bilateral hearing loss! From a clinical perspective we may have goals such as improving hearing or reducing the experience of disability, but clients will typically be focused on the intervention as a means to an end.
As we know, they will report stories and anecdotes about problems that have arisen for them – such as being on the telephone and having no idea that they were talking to their boss. Or ringing a workplace and speaking intimately with the person on the other end of the telephone, only to realise that it was not their partner. Then there are the problems at home (the misunderstandings, the confusions, the yelling perhaps, the volume of the TV) and those experienced in social settings (hearing in group settings, at the cinema, social gatherings).
“The dynamics of misperception and reluctance are such that they can readily impact on the capacity of an individual to understand how hearing is affecting their life.”
The more insightful client may even be able to talk about how these situations leave them feeling, how hearing impairment impacts on their quality of life or satisfaction with what they might be achieving in life overall. Unfortunately, some two thirds of our clients lack insight into the effects of hearing impairment in their daily life. The dynamics of misperception and reluctance are such that they can readily impact on the capacity of an individual to understand how hearing is affecting their life [1]. It is for reasons such as this that people often mistake the onset of impaired hearing for interpersonal conflicts or life style changes.
Overcoming challenges to client-centred evaluation
While these factors are not new to the experienced audiologist or hearing therapist, they do create distinct challenges for the evaluation of hearing services, because all clients do not begin their clinical interaction with you with the same ‘social’ baseline. In one sense, in an era of client-centred and outcomes based therapy, evaluations need to be tailored to the client. However, some evaluative processes (e.g. the use of the COSI [2]) assume a reasonably educated client, or the allocation of sufficient clinical time to educate the client so that they can make informed decisions about the goals of their hearing services programme. Worst still, effective interventions, such as those that actually educate the client about their hearing impairment, may produce evaluative results which on face value at least, suggest that the client is actually worse off for the experience of seeing us! Of course, this is typically not the case, but care is required in using and interpreting outcomes based evaluations in hearing services.
Importantly, the research shows two things. First that as a result of effective interventions, clients are often enabled to make more realistic assessments of the impact of hearing impairment in their lives. Second, and as a result of the interventions provided, they are more able to effectively manage the difficulties that they encounter and their quality of life improves [3, 4].
This background information then offers up some quite distinct challenges to the effective measurement of efficacy in the audiological setting. Three needs are evident. First, our evaluation protocols need to be sufficiently comprehensive so as to be able to capture information on a range of indicators (e.g. client enablement, resolving social difficulties, enhancing wellbeing and life satisfaction, addressing family needs). They need to be sufficiently parsimonious that clients can easily complete them in the waiting room; and finally, they need to serve some useful clinical purpose.
Easier listening protocols
One protocol that sets out to address these challenges is the Easier Listening Program’s set of evaluation tools [5]. These tools were developed from a combination of the most salient questions from the initial evaluations of the Montreal Hearing Health Program [3, 4], combined with basic questions about quality of life, device use and the like. The evaluation tools come in a pre-post format and they can be used in evaluation designs taking repeated measures over time (e.g. baseline, three months, six months post fitting etc.). They can quickly and easily be completed by clients prior to seeing a clinician and can also be used to guide initial needs assessment, client counselling, motivational sessions and the management of client expectations.
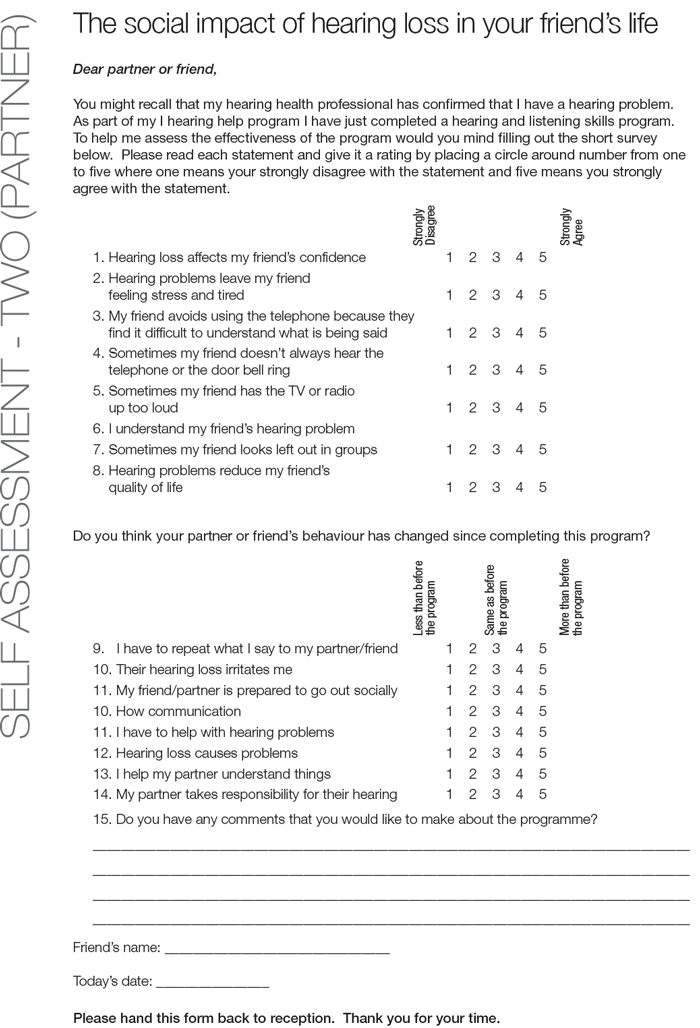
Figure 1. Easier Listening Program self-assessment forms.
An example of one of the assessment forms can be seen in Figure 1. The form has two basic sections. The first section is made up of responses from the client perspective, to identify the kinds of difficulties the client may be experiencing as a result of their perceived hearing impairment. As such they serve as a client’s base line experience. Second, as the client is asked to have a similar form completed by a significant other, the form provides an opportunity for input from someone who knows them well. Combined, the two perspectives assist the clinician in exploring the nature and extent of client difficulties and experiential insight.
Counselling strategies easily arise from insights offered on the form. For example, if a person reports that hearing impairment has reduced their confidence, the clinician may ask the client to share an example of when this problem may have arisen. Used as a counselling tool, the client and significant other form may also facilitate developing client insight into the nature and impact of their hearing difficulties, as experienced by others, and as such, potentially serve as a motivational counselling tool.
Comparatively assessing the two forms together, within the clinical setting, is quite straightforward. If both people indicate that something is a problem, then we accept it as problem. If both people indicate that something is a not problem, then we accept that it probably isn’t a major problem in this instance. If only one person suggests that something is a problem, then we explore this issue with regards the extent to which the individual was aware of the issue for the other and to explore the extent to which they would want to learn more or to do something about the issue, simply to help the other person. The clinical door, as it were, swings both ways here. For example, a client may not readily acknowledge that they have the TV up too loud, while a partner may not realise that hearing impairment has reduced their partner’s confidence. Rehabilitation strategies are available to assist clients and significant others address these challenges.
“Process evaluation tells us what it is about our intervention that is associated with the change process.”
From an evaluation perspective, these first seven questions provide information that assists with process evaluation. Process evaluation tells us what it is about our intervention that is associated with the change process. The use of these forms enables the monitoring of a range of change processes. A partner might realise, for example, how hearing impairment impacts on the client, and in turn support them more in difficult social settings. Effective rehabilitation may also enable the client to gain coping skills to manage their hearing impairment and as such feel more confident in social settings. Clients may come to realise that they are more left out of social settings than they realised or begin to notice people complaining more. These are positive outcomes, even if the scoring of the item seems negative.
Importantly, the first seven items are also assessed in the context of the last two items – their self-rating of quality of life and their self-rating of the extent to which they feel that they can manage their hearing and listening difficulties. At a population level, people typically score a rating of 7 or more, out of 10, for quality of life [6]. Hearing impaired people typically score lower. As such, as a result of an effective hearing rehabilitation programme, one would expect that the client’s self-rated quality of life score would increase, certainly by the six month follow up [7]. By contrast, given growing client awareness and competency-based rehabilitation interventions, the client’s self-rated ability to manage their hearing difficulties may vary over time, perhaps initially falling by the three-month evaluation point (due to increased awareness) before rising again by the six-month mark, as a result of effective rehabilitation and time for behaviour change. In addition to providing useful evaluation tools, follow-up evaluations also provide opportunities for further counselling and client education as they enable the identification of concrete difficulties which clients may have not yet resolved.
Concluding remarks
It is important, particularly in an era of outcomes-based evaluation [1], that hearing services do not over-promise on what can be delivered. Our work is centred on the optimal use of technology in the management of reduced hearing sensitivity and the provision of rehabilitation services aimed at reducing the experience of hearing disability. While hearing services may serve to enhance people’s quality of life, the services in and of themselves cannot overcome problems associated with factors such as discrimination, be it in the community or in the workplace. To this end, should clients be seeking further improvements to their wellbeing, referrals to appropriate health or social services may be indicated. And while we may skill clients to the best of our abilities, specific factors impacting on social inclusion (e.g. community awareness of hearing impairment, or the acoustic accessibility of public spaces) may require social rather than clinical initiatives.
References
1. Hogan A. Engaging in change at a personal level. In: Hogan A, Phillips R, (Eds.). Hearing impairment and hearing disability – towards paradigm change in hearing services. London, UK; Ashgate; 2015:85-104.
2. National Acoustic Laboratories. Client Oriented Scale of Improvement. 2016;
https://www.nal.gov.au/wp-content/uploads/
sites/3/2016/11/COSI-Questionnaire.pdf
Last accessed November 2017.
3. Getty L, Hetu R. Development of a rehabilitation program for people affected with occupational hearing loss. 2. Results from group intervention with 48 workers and their spouses. Audiology 1991;30:317-29.
4. Hogan A, Ewan C, Noble WG, Munnerley G. Coping with occupational hearing loss: the University of Montreal Acoustics Group rehabilitation programme. An evaluation study. Journal of Occupational Health and Safety 1994;10(2):107-18.
5. Hogan A. Easier Listening – Strategies for living with partial hearing loss. Canberra, Australia, EGA Insights; 2008. Download from Anthony’s page on academia.edu. Includes copies of the outcomes measures.
6. Australian Unity Wellbeing Index 2016.
https://www.australianunity.com.au/
media-centre/news-and-media/
australian-unity-wellbeing-index-2016
Last accessed November 2017.
7. Hawthorne G, Hogan A, Giles E, et al. Evaluating the health-related quality of life effects of cochlear implants: a prospective study of an adult cochlear implant program. International Journal of Audiology 2004;43:183-92.





