Introduction
Patient-centred care in the health sector is a worldwide concern [1, 2]. Patient-centred rehabilitation is characterised by availability, appropriateness, preference, and timelines [3]. A consensus report by the Institute of Medicine [4] defines a patient-centred approach as ‘providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions’.
The British National Institute for Health Care Excellence (NICE) and the World Health Organisation (WHO) have both addressed the implementation of patient-centred rehabilitation. NICE emphasises that “to develop a successful strategy for change, you need to understand the types of barriers faced in healthcare” [5]. Despite the on-going discussion on Person Centred Audiological Rehabilitation (PCAR) and the need to identify barriers, there is a lack of a systematic global investigation of the perceived obstacles for implementing PCAR from the practitioners’ viewpoint [6].
Aim
The underlying goal of the study is to enable the development of strategies and practical tools to overcome existing barriers to change, thereby making PCAR the benchmark in daily clinical practice. The aim of this article is to determine the most important hindering and facilitating factors for implementing a PCAR perceived by practitioners.
Methods and materials
Based on the conviction that there is a need to develop a proactive approach to change Audiological Rehabilitation (AR) towards patient-centred rehabilitation, the IDA Institute [7] dedicated its 2012 seminar series to the topic of ‘managing change’. As a pre-assignment, participants at the 2012 IDA Seminar were asked to write a list of facilitating and hindering factors they had experienced in applying a patient-centred approach in their clinics, which yielded approximately 40 descriptions of such factors. Ten factors were established. Each factor can be recognised as either a hindering or a facilitating factor or both. The 10 factors were Personal Factors, Patient Perspective, Staff Knowledge, Workplace Culture, Resources, IDA Motivation Tools [7], Relationships between different professions, Regulations / rules, Management and Technological Focus, Hearing aids.
“Providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.”
The questionnaire was distributed in November 2012 (web survey) to all members of the IDA community. Two reminders were sent out, and on 31 January 2013, a total of 209 valid questionnaires had been returned. These questionnaires formed the basis of the analysis [8].
Result
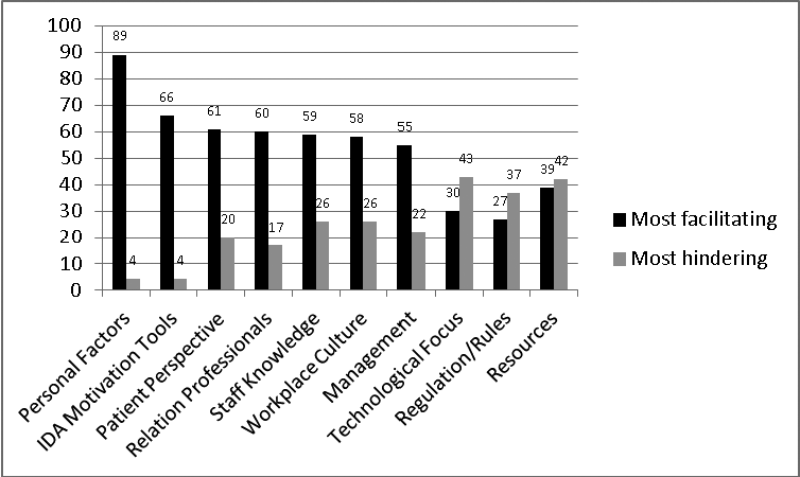
Figure 1 shows that Personal Factors was the single most important facilitating factor. The second most facilitating (or less hindering) factor was IDA Motivation Tools. Regarding these two factors, the respondents’ experiences were unambiguous: 89% experienced Personal Factors as facilitating vs. 4% who experienced it as hindering and 60% experienced IDA Motivation Tools as facilitating vs. 4% who experienced it as hindering. At the other end of the spectrum, three factors seemed to be less facilitating than the other factors: Technological Focus, Regulations / rules and Resources. However, the respondents’ experiences were very different; Technological Focus was 30% facilitating vs. 43% hindering, Regulations / rules was 27% facilitating vs. 37% hindering, and Resources was 42% facilitating vs. 39% hindering (Figure 1).
Figure 1: The most facilitating and the most hindering factors (%).
Discussion
The fact that Personal Factors was the most important factor indicates that an important vehicle for change towards PCAR is engaging staff members with a passion for PCAR to thrive. In the literature on organisational change, this aspect is commonly mentioned as one of the most important aspects of implementing organisational change. For instance, from a management perspective, it is important to take advantage of such persons in the organisation and to empower employees to take the role of change agent. It is also important to give these people possibilities in terms of recourses and adequate tools to implement their visions. The second most important facilitating factor was IDA Motivation Tools. Having the ambition to implement PCAR is not sufficient because one needs scaffolds. The tools developed by the IDA Institute are just one example of tools that can be used. The tentative conclusion is that it is important to provide staff with supportive and appropriate tools when implementing PCAR. There were also a number of other factors that a majority of the respondents perceived as facilitators. The presence of Professional Relations, Staff knowledge, Workplace culture and Management in this list indicates the importance of internal clinician aspects, which is in accordance with previous findings that suggest that a safe, supportive, inclusive, and collaborative culture needs to be established.
The most hindering factors referred to structural conditions. Resources and Regulations / rules were among the most hindering factors. The important conclusion is that the implementation of PCAR must be preceded by an investigation of the structures of rules that regulate practice; in addition, at least initially, resources must be available. These findings are important. In the mainstream literature of organisational change, much focus has been placed on individual aspects.
The Technological Focus was also reported to be a significant hindering factor, although the opinion was quite dichotomous. The question about this aspect was referring to circumstances in which a technological focus at the workplace might hamper the understanding of and willingness to implement patient-centred care. The findings here indicate that a need for approaches that extend rehabilitation beyond technology alone still exists.
Implications of the study
One important implication for change is that structural issues must be dealt with at the policy and management levels. A change process that builds on capabilities and potentiality among staff is another significant aspect. This process requires training that includes scaffolding, such as those developed by the IDA Institute [7]. Finally, the data indicate that some respondents experience factors as hindering that others experience as facilitating. This dichotomy indicates that there is a need for benchmarking, taking into account the experiences of those who have successfully implemented PCAR.
This work was funded by a grant from the IDA Institute, Denmark, and by Örebro University, Sweden.
References
1. World Health Organization (WHO) 2003. Adherence to long-term therapies. Evidence for action.
2. World Health Organization (WHO). Regional Office for Europe. 2012. Engage in the Process of Change; Facts and Methods.
3. Berry LL, Seiders K, Wilder SS. 2003. Innovations in access to care: a patient-centered approach. Ann Intern Med 2003;139:568-74.
4. Institute of Medicine (IOM). Crossing the quality chasm: A new health system for the 21st century. Washington, DC, USA; National Academy Press, 2001.
5. National Institute for Health and Clinical Excellence. 2007. How to change practice. Understand, identify and overcome barriers of change. www.nice.org.uk Last accessed July 2014.
6. Grenness C, Hickson L, Laplante-Lévesque A, Davidson B. 2014. Patient-centred care: A review for rehabilitative audiologists. Int J Audio. 2014;53:S60-7.
7. IDA Motivation Tools consist of three tools (the line, the box, and the circle) and provide guidance on appropriate communication strategies that direct a change process in the most efficient way.
http://idainstitute.com/
tool_room/tools/motivation_tools
Last accessed July 2014. See also the WHO (2012, Chapter 4).
8. IDA Institute. 2013.
http://idainstitute.com/events/
seminars/managing_change/
Last accessed July 2014.
Declaration of Competing Interests: BD was among the faculty that organised a seminar that focused on Person-centered Audiological Rehabilitation. IDA Institute financed the study.