Another pill to cure the ill? Alec Lapira discusses the warning signs of polypharmacy in the elderly population.
Polypharmacy in the elderly
Polypharmacy – defined as the use of five or more medications – occurs in 20–37% of older people [1]. The characteristic hallmark of ageing in physiological terms is reduced adaptive capacity. Elderly patients with decreased plasma volume, diminished vasomotor regulation, impaired glucose tolerance and greater morbidity from disease are more vulnerable to adverse effects of drugs.
Treatment of elderly patients can be complex due to multiple illnesses and drug therapies that can produce adverse drug reactions (ADRs), especially if receiving multiple medications. One study showed that elderly women took an average of six prescription drugs and three over-the-counter drugs concurrently [2].
“The toxicity of drug combinations may sometimes be synergistic and be greater than the sum of the risks of toxicity of either agent used alone.”
It has been clearly shown that the risk of ADRs (including interactions) is related to the number of medicines taken, and that the elderly receive more medicines, sometimes inappropriately. Risk factors include the prescribing doctor, patient age and co-morbidity. Polypharmacy is associated with several negative outcomes. The risk of ADRs is increased 3-4 fold in 81% of patients on six or more medications [3]. The toxicity of drug combinations may sometimes be synergistic and be greater than the sum of the risks of toxicity of either agent used alone. The risk of falling is doubled with four or more medications [4]. Furthermore, prescribing errors increase from 15% with one medication to 35% with four or more medications [5].
Rationale for prescribing in older people
The evidence base for prescribing to frail older people is small and disproportionate to the level of prescribing. Only 3% of randomised, controlled trials and 1% of meta-analyses are published about people over 65 years of age [1]. Yet, the proper use of medications is perhaps the single most important strategy in the care of elderly patients. There is evidence that elderly patients often are prescribed inappropriate medications and, as a result, tend to have more frequent and often serious adverse effects. Unfortunately, cost also frequently plays a role in selection of medications. Physicians are often bound by formularies that may limit access to the safer, but often more expensive, medications. Optimal drug therapy is paramount in treating acute illness, maintaining health, and preventing further decline, which all represent the benchmark of geriatric care and successful ageing [6].
Adverse drug reactions (ADRs)
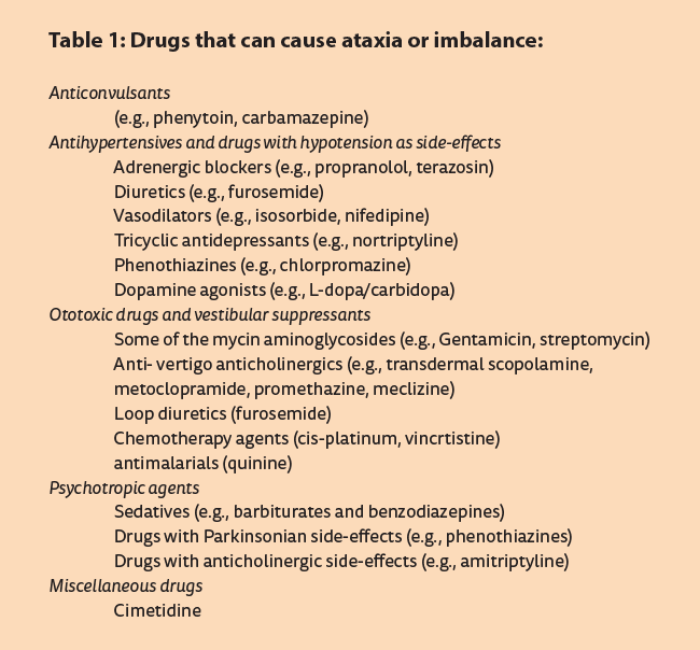
Though marketing and guideline protocols tend to focus on evidence of efficacy, physicians should also consider the impact of ADRs in older people, who are four times more likely to be admitted to hospital as a result of an ADR; whereas 50% of adverse reactions in older people can be avoided by judicious prescribing [5]. Most clinicians and patients assume that only prescription drugs have risks of adverse reactions, but over-the-counter medications can also be harmful. While 80% of drug-related adverse effects are due to prescription medications, the remainder is caused by over-the-counter drugs. The risk of an adverse drug reaction increases with every new drug added to the treatment regimen [7]. Medications are a common contributor to dizziness and ataxia (see Table 1) as elderly patients are often on multiple drugs [8]. In fact, medications are the most common cause of symptomatic orthostatic hypotension as well as hypoglycemia.
In the elderly, symptoms of an adverse drug reaction can be extremely subtle and may manifest as increased falls, confusion, sedation, constipation, urinary retention, decreased oral intake, or a general failure to thrive. Because these problems are commonly seen in geriatric practice, it is not uncommon for a physician to ‘treat’ an ADR with another drug [2].
Drug monitoring
Because the rate of adverse drug reactions is substantial, it is important to monitor older patients on drug therapy closely. When adverse drug reactions occur, they tend to be severe and less likely to be recognised or reported by the patient. Medications should be prescribed only for appropriate reasons, discontinued when they no longer provide benefit, and dosed correctly to reflect alterations in age-related pharmacokinetics and pharmacodynamics.
“Medications should be prescribed only for appropriate reasons, discontinued when they no longer provide benefit, and dosed correctly to reflect alterations in age-related pharmacokinetics and pharmacodynamics.”
Healthcare professionals need to be especially vigilant for falls and confusion. The risk of falling is increased by 71% in older people taking psychotropic medications [4]. Benzodiazepines are associated with a 50% increase in the rate of hip fractures [9].
Medications cause 11–30% of cases of delirium and 2–12% of cases of chronic confusion or dementia in the elderly [10]. Although anticholinergic drugs and psychotropic drugs are common culprits, any drug should be considered. A pitfall to avoid is the practice of prescribing additional medication to counter the adverse effects of drugs; the ‘prescribing cascade’. For example, gout therapies are commonly prescribed in users of thiazides, and levodopa to patients taking metoclopramide [11].
Withdrawing medications
Healthcare practitioners have been encouraged to withdraw medications in their older patients with polypharmacy [5]. Withdrawing medications is difficult with enormous marketing pressures to maintain high levels of prescribing. There is evidence for the benefit of reducing medications in elderly subjects with polypharmacy. In a placebo controlled withdrawal trial of psychotropic medications in older subjects taking on average more than five medications, there was a substantial reduction in falls [12]. There have been at least four trials investigating the effect of withdrawal of antihypertensive medications in older people and overall, 40% of subjects remain normotensive [13].
Most drugs can be stopped without major withdrawal effects. However, abrupt withdrawal of benzodiazepines can be associated with seizures, beta blockers with tachycardia and exacerbation of ischaemic heart disease, and levodopa with neuroleptic malignant syndrome [14].
Conclusion
The decision to prescribe a medication to an older patient should be guided by principles of:
- Self-sufficiency – frail older adults may often be concerned about issues of autonomy and side effects of medications, rather than whether their disease or risk factor is managed according to the latest published guidelines.
- Efficacy – there is little evidence for benefit of most pharmacotherapies in frail, older people with comorbidity and multiple medications. Evidence for efficacy is often predicted and based on studies on younger patients.
- Adverse drug reactions – more common in older people and a frequent cause of morbidity and mortality. Polypharmacy exacerbates this problem. The high rate of adverse drug reactions should be balanced against the often uncertain efficacy evidence in older people before a decision to prescribe is embraced [8].
- Drug tuning: treatment begins by removing unnecessary agents and drug ‘tuning’, or substituting similar, but better tolerated, medications. For example, an H2 blocker which does not cross the blood-brain barrier, such as ranitidine, may be better tolerated than one that does, such as cimetidine.
- Drug monitoring - attributing signs and symptoms associated with ageing, such as weakness, confusion, anorexia, anxiety, and memory loss, to old age, rather than suspecting the effects of drugs, should be avoided. This is especially true if patients are receiving hypnotic, antidepressant, antianxiety, or anticholinergic medication.
- Education - polypharmacy has an origin in patients’ belief that they need a pill for every ill. Lack of knowledge of what is caused by normal ageing versus disease may lead to unnecessary medication. For example, insomnia in an older adult may be due to normal sleep variation with ageing. Explaining these changes and reviewing sleep hygiene may be sufficient treatment. Prior to educating patients, healthcare professionals must have the necessary knowledge and understanding of these principles. It is the awareness of such interactions that is important rather than the absolute avoidance of co-prescriptions of potentially interacting drugs. Rational prescribing can: reduce the number of prescribed medicines; reduce the potential for interaction between remaining prescribed medications; and identify and make allowances for over-the-counter medicines.
The use of the lowest dosage of as few drugs as possible should be the cardinal rule.
References
1. Nair BR. Evidence based medicine for older people: available, accessible, acceptable, adaptable? Aust J Ageing 2002;21:58-60. 2. Wilcox SM, Himmelstein DU, Woolhandler S. Inappropriate drug prescribing for the community-dwelling elderly. JAMA 1994;272:292-6.
3. McLean AJ, Le Couteur DG. Aging biology and geriatric clinical pharmacology. Pharmacol Rev 2004;56:163-84.
4. Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 1999;47:30-9.
5. Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. J Pharm Pract Res 2003;33:323-8.
6. Monane M, Monane S, Semla T. Optimal medication use in elders: key to successful aging. In: Successful Aging. West J Med 1997;167:233-7.
7. Beers MH, Ouslander JG, Fingold SF, et al. Inappropriate medication prescribing in skilled-nursing facilities. Ann Intern Med 1992;117:684-9.
8. Turnheim K. Drug dosage in the elderly: is it rational? Drugs Aging. 1998;13:357-79.
9. Cumming RG, Le Couteur DG. Benzodiazepines and hip fractures in older people: an evaluation of the relationship. CNS Drugs 2003;17:825-37.
10. Moore AR, O’Keeffe ST. Drug induced cognitive impairment in the elderly. Drugs Aging 1999;15:15-28.
11. Rochon PA, Gurwitz JH. Optimising drug treatment for elderly people: the prescribing cascade. Br Med J 1997;315:1096-9.
12. Campbell AJ, Robertson MC, Gardner MM, et al. Psychotropic medication withdrawal and a home based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc 1999;47:850-3.
13. Froom J, Trilling J. Reducing antihypertensive medication use in nursing home patients. Arch Fam Med 2000;9:378-83.
14. Boockvar K, Fishman E, Kyricou CK, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long term care facilities. Arch Intern Med 2004;164:545-50.
Declaration of Competing Interests: None declared.
ABOUT THE AUTHOR
Dr Lapira is an ENT Specialist and an Audiological-Vestibular Physician working at St James & Capua Hospitals, Malta with over 20 years of clinical experience. He lectures on voice & ENT disorders at the University of Malta and serves as adjunct Professor in Audiology at Nova Southeastern University of Fort Lauderdale, Florida. He is also a board member of the EU-appointed TINNET group, tasked to standardise guidelines for the management of tinnitus across the EU member states.