Fiona Barker explains the importance of recognising and understanding how habitual behaviours in vestibular patients can affect treatment outcomes, and how we as audiologists can support and encourage patients to modify these behaviours and perhaps address our own professional behaviours in the process.
The importance of behaviour
Behaviour can be defined as ‘anything a person does in response to internal or external events’. Behaviours are therefore physical processes that occur in the body and are controlled by the brain [1]. The way that people behave plays a key role in determining health outcomes and quality of life. Figure 1 shows how behaviour in any particular context can interact with cognitive and emotional response to mediate outcome.
Cognition and emotion can both determine behaviour and behaviour can influence cognition and emotion. However, ultimately it is behaviour that directly influences outcome in this model. As clinicians we see this every day. People may understand the need to change their behaviour and be unhappy with their current situation but it is only when this is translated into action that the outcome will change. Despite the importance of health as an outcome for most people, figures from the Department of Health and the King’s Fund suggest that the majority of the adult population engages in at least one behaviour likely to put their health at risk.
“The way that people behave plays a key role in determining health outcomes and quality of life.” “We could and should be using behavioural models and theories to ensure that our patients have the capability, opportunity and motivation to engage in appropriate management be that rehabilitation, medication or lifestyle changes.”
People continue to smoke, drink alcohol to excess, eat too much of the wrong things and not take enough physical exercise. The same is true of vestibular patients. They want to feel better but they frequently engage in behaviour that works against that: they avoid head movements or particular environments; they continue taking vestibular sedatives; they do not make changes in their diet or other lifestyle changes that might reduce their symptoms. To improve our patients’ vestibular health we often need to help them change their behaviour. To do this we need to first understand their behaviour. We need to understand why they are behaving as they are; what is going on, what has caused it and what is maintaining it and then use this as a base for understanding what needs to change in order for them to reduce or manage their symptoms more effectively.
Understanding behaviour
A first step in understanding behaviour is to define the problem in behavioural terms. High rates of falls in the elderly is a recognised problem but the behavioural issue is the low levels of physical activity which can lead to increased fall risk in this population.
Second, it is important to recognise that behaviour does not occur in a vacuum. In the simplified diagram in Figure 1, behaviour is shown as a single box. However this is not the case in reality. In reaching a judgement about how to intervene to improve outcome it is important to have a full picture of how different players within a behavioural system interact. For example, evidence suggests that healthcare professional behaviour interacts with patient behaviour to influence outcome. This is embodied in frameworks such as the chronic care model [2]. In a complex system like healthcare, it therefore becomes necessary to understand not only patient behaviour but also the behaviour of the individuals and organisations with whom the patient interacts.
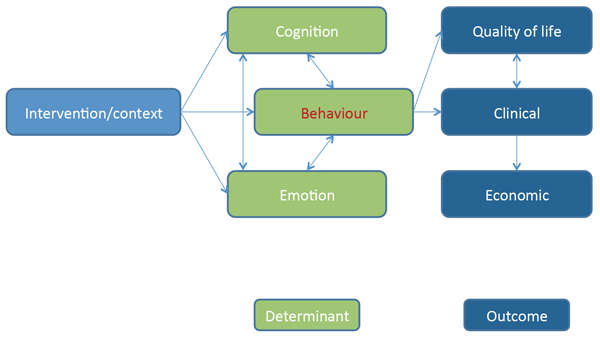
Figure 1: Causal model of behaviour.
A clear behavioural specification and mapping of the problem will lead to a better analysis of who needs to do what differently, when, where and how for change to occur.
Use of theory
Those of us working in healthcare are practical. We want to help people. The strong temptation is to move from identifying a problem straight to trying a solution. Unfortunately this can lead to what some have called ISLAGIATT intervention development: that is, ‘It Seemed Like A Good Idea At The Time’[3]. Sometimes these interventions work but, with no underlying theory, it is very difficult to work out whether they could have worked even better, why they worked or, if they didn’t, why not.
Theory can be defined as ‘a supposition or a system of ideas intended to explain something’. An appropriate theory may therefore be useful in explaining behaviour in a particular context. Theory can guide our understanding of what needs to change and then how to change it. Interventions developed using theory are more likely to work. Systematic application of criteria such as likely impact, likely ease and cost of implementation and spillover effects on other behaviours and people can guide the choice of where to intervene based on a thorough theoretically-based understanding of the behavioural problem and it’s context. In addition, theory can be used to evaluate existing interventions to work out why things worked or did not work so that it is possible to move forward in making interventions more effective and to judge whether interventions can be generalised between contexts [1,3,4]. However, there are many theories of behaviour change often with overlapping, but differently named, constructs [1].
In addition, there is little guidance on how to choose an appropriate theory for a particular context [5]. This diversity and complexity has been cited as a potential reason why theory is under-used in intervention design and evaluation making replication, implementation, evaluation and improvement more difficult [4,5]. Researchers argue that there is a need for a comprehensive model of behaviour applicable across contexts.
Michie et al. [1,5] propose that people need the capability (C), opportunity (O) and motivation (M) to perform a behaviour (B) and developed the COM-B model to guide understanding of behaviour in context and develop behavioural targets as a basis for intervention design. The model provides a simple starting point and can signpost to specific psychological theories of, for example, motivation if a more granular theoretical understanding of behaviour is required.
Importantly, this model has also been embedded within a guide for intervention development called the Behaviour Change Wheel (BCW) that allows the clinician or researcher to move in a systematic way from problem specification and analysis through to intervention design and evaluation right up to implementation. Figure 2 shows the principle components of the BCW.
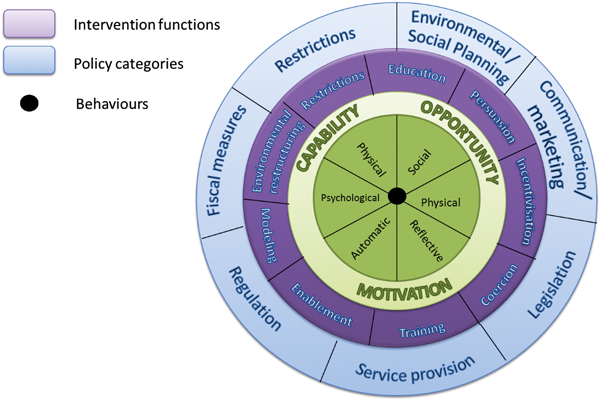
Figure 2: Behaviour change wheel.
The COM-B model and BCW are currently being used across behavioural contexts, inside and outside healthcare. In hearing healthcare, it has been used to guide the development of an intervention that aims to improve hearing aid use. It has not yet been used in the context of vestibular care so the field is wide open.
In summary, we could and should be using behavioural models and theories to ensure that our patients have the capability, opportunity and motivation to engage in appropriate management be that rehabilitation, medication or lifestyle changes. We can also use it to look at our own individual professional behaviour and service provision more widely and analyse whether we have the capability, opportunity and motivation to provide evidence-based care that meets the needs of our patients.
References
1. Michie S, Atkins L, West R. The behaviour change wheel: A guide to designing interventions. 1st Edn. London, UK; Silverback; 2014.
2. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775-9.
3. Strauss S, Tetroe J, Graham ID (Eds). Knowledge translation in health care: moving from evidence to practice. Hoboken, NJ, USA; John Wiley & Sons; 2013.
4. Eccles MP, Grimshaw JM, MacLennan G, et al. Explaining clinical behaviors using multiple theoretical models. Implement Sci 2012;7:99.
5. Michie S, van Stralen MM, West R. 2011. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42.
Declaration of competing interests: None declared.
You can find out more about the COM-B model and Behaviour Change Wheel at the Centre for Behaviour Change at UCL (www.ucl.ac.uk/behaviour-change).




