Introduction
Early identification of hearing loss in infants followed by prompt intervention is well established as the key to maximising the development of speech, language and psychosocial skills. Many countries have already adopted early hearing detection and intervention (EDHI) programs, some for more than 20 years, and have met with good success. However, there are areas that need both development and refinement to fulfil the mandate for provision of services to infants with permanent sensory, conductive and neural losses, as set out by the Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs: Joint Committee on Infant Hearing:
“…audiologists provide comprehensive audiological diagnostic assessment to confirm the existence of the hearing loss, ensure that parents understand the significance of the hearing loss, evaluate the infant for candidacy for amplification and other sensory devices and assistive technology, and ensure prompt referral to early intervention programs. For the treatment and management component, audiologists provide timely fitting and monitoring of amplification devices.” [1]
The utilisation of cortical auditory evoked potentials (CAEPs) in infants are under investigation to address two specific areas:
- validation of the benefits of amplification in terms of detection and discrimination of speech sounds for all types of hearing loss including neural disorders, e.g. auditory neuropathy spectrum disorder (ANSD)
- estimation of hearing thresholds in infants with ANSD; the auditory brainstem response (ABR) cannot provide meaningful information regarding sensitivity at different frequencies important for speech understanding for this subset of infants.
Validation of hearing aid benefit
Early speech reception skills rely on an infant’s ability to detect the presence of speech sounds with varying spectral content and to discriminate subtle differences between meaningful speech contrasts. Although information gained from early diagnostic ABR testing (ear and frequency-specific) and hearing-aid fitting verification (real-ear probe measures) assists clinicians in the provision of audible speech, objective validation of auditory function is difficult to accomplish in the early months of life. The utilisation of CAEPs holds promise to assess both detection and discrimination of speech sounds.
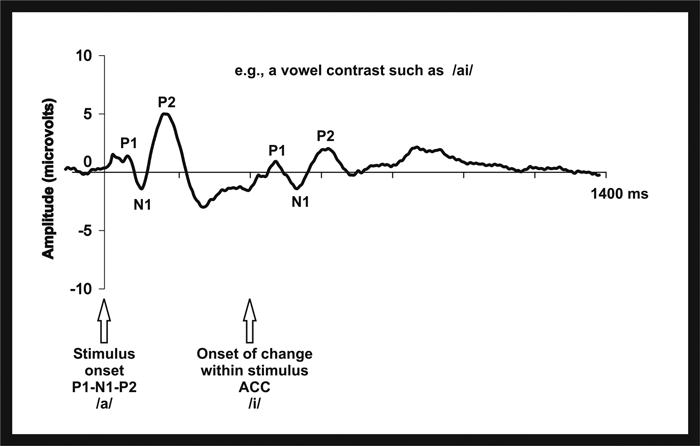
Figure 1: Representation of a typical CAEP onset response and acoustic change complex.
CAEPs are long-latency recordings of the EEG elicited by different types of auditory stimuli (e.g. tones, noise, speech). CAEPs can be elicited by the onset of a stimulus, the slow cortical response or the P1-N1-P2, and to a change within a stimulus, the acoustic change complex (ACC) as shown in Figure 1. The P1-N1-P2 is used clinically to estimate adult thresholds when an objective measure is needed (e.g. compensation cases) because it can be recorded at near-threshold levels. The ACC has potential for use clinically because it can be elicited to speech contrasts, an area primarily investigated in adults. These potentials can be recorded in infants but there are maturational differences in the characteristics of the response (morphology, amplitude and latency) and many fewer studies. There are also differences in the CAEP when the infant is awake versus asleep; however, the present discussion will focus only on the former.
Highlights from the data thus far…
Detection:
- CAEPs can be elicited to speech stimuli in most infants with normal hearing and hearing loss (unaided and aided) but 25% of infants with hearing aids do not exhibit a CAEP when audibility is expected [2]
- There are stimulus-related issues when recording aided CAEPs: (i) hearing-aid processing effects can result in changes to stimulus onset characteristics which in turn alter the CAEP [3] (ii) signal-to-noise ratio can also determine the characteristics of the CAEP [4]
- CAEP amplitude is only related to audibility for a limited range of stimulus levels in normal-hearing infants [5]
- Stimulus duration and ISI can be as short as 31 and 750ms, respectively, without significant changes in amplitude – saves testing time [6].
Clinical implications
- The presence of a CAEP can be interpreted as auditory information reaching the auditory cortex; however, does not predict where the speech stimulus fits within the infant’s dynamic range.
- The absence of a CAEP is not easily interpreted.
- The ability to record CAEPs in infants to short-duration stimuli and short inter-stimulus intervals supports the clinical feasibility of recording this response in the clinic.
Future directions
Further research is needed to explain why cortical responses are not elicited in aided infants when responses are expected.
Discrimination:
- One study with a small group of young children with normal hearing and hearing loss (unaided and aided) has demonstrated that ACCs can be elicited to changes in vowel pairings [7]
- Promising results for ACCs elicited to contrasting English and Hindi consonant-vowel (CV) pairs have been reported for normal-hearing infants when the stimulus duration for each CV was long (410ms); results are less consistent for a shorter duration (256ms) [8].
Clinical implications
Preliminary unaided and aided ACC findings support further study but this measure is not yet ready for clinical use.
Future directions
More infant ACC studies are needed to determine which stimuli and recording parameters would be optimal for assessing hearing-aid benefit for a range of hearing losses.
Estimation of hearing thresholds in cases of ANSD
For infants with ANSD, ABR findings contribute to the identification of the disorder but do not provide estimation of hearing thresholds. Without an accurate objective measure of hearing thresholds, fitting of amplification and informing the parent of the status of their child’s hearing are delayed until approximately six to eight months of age. The CAEP has a technical advantage over the ABR – it is much less reliant on synchronised nerve firing – this means that cortical responses will often be present in an individual who has temporal processing difficulties (e.g. ANSD) when an ABR response is absent or grossly abnormal. The presence of a response confirms that auditory input was detected and processed at the level of the cortex.
Highlights from the data thus far…
- Rance and colleagues [9] first showed that CAEPs can be recorded in children with ANSD and that the thresholds estimated correlate well with behavioural findings (unaided and aided); however, they also noted that the presence of CAEPs and degree of hearing loss did not predict speech perception ability [9]
- Recent work suggests that ACCs recorded to gaps in continuous noise, a measure of temporal processing essential to perceive speech, correlate strongly with word recognition ability in children with ANSD who have cochlear implants [10].
Clinical implications
- CAEPs can be used to estimate hearing thresholds in children with ANSD for the purpose of fitting hearing aids
- ACCs to gaps in noise can be used to predict word recognition ability in children with ANSD who us cochlear implants
Future directions
More research is needed for infants with ANSD using the CAEP onset response to confirm the accuracy of this measure for the estimation of hearing thresholds; similarly, the ACC to gaps needs to be explored for accuracy and clinical feasibility for the prediction of word recognition ability in infants.
Conclusion
Although on-going research is needed to fill the gaps in our knowledge about recording CAEPs in infants, the findings to date show promise for the CAEP as an objective measure for validation of hearing device benefit, and the estimation of hearing thresholds and prediction of speech perception ability in infants with ANSD.
References
1. American Academy of Pediatrics, Joint Committee on Infant Hearing Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007;120:898-921.
2. Van Dun B, Carter L, Dillon H. Sensitivity of cortical auditory evoked potential detection for hearing-impaired infants in response to short speech sounds. Audiology Research 2012;2:e13.
3. Jenstad LM, Marynewich S, Stapells DR. Slow cortical potentials and amplification – Part II: Acoustic measures. Int J Otolaryngol;epub 2012 Oct 31.
4. Billings CJ, et al. Clinical use of aided cortical auditory evoked potentials as a measure of physiological detection or physiological discrimination. Int J Otolaryngol;epub 2012 Oct 8.
5. Purdy SC, et al. Stimulus level effects on speech-evoked obligatory cortical auditory evoked potentials in infants with normal hearing. Clin Neurophysiol 2013;124(3):474-80.
6. Golding M, et al. The effect of stimulus duration and inter-stimulus interval on cortical responses in infants. Aust N Z J Audiol 2006;28:122-36.
7. Martinez AS, Eisenberg LS, Boothroyd A. The acoustic change complex in young children with hearing loss. Semin Hear 2013;34(4):278-87.
8. Small SA, Werker JF. Does the ACC have potential as an index of early speech-discrimination ability? A preliminary study in 4-month-old infants with normal hearing. Ear Hear 2012;3:e59-69.
9. Rance G et al. Speech perception and cortical event related potentials in children with auditory neuropathy. Ear Hear 2002;23(3):239-53.
10. He S et al. Objective measures of electrode discrimination with electrically evoked auditory change complex and speech-perception abilities in children with auditory neuropathy spectrum disorder. Ear Hear 2014;May-Jun;35(3):e63-74.
Declaration of competing interests: None declared.




