Children and parents like the reassurance that staying under the care of the team who looked after them from birth gives, but as the child approaches adulthood he / she must come under the care of a new team. This can be a fraught and worrying time. Jacqui Rogers and Dr Lynda Brook provide good practical advice for parents and doctors.
Adolescence is an exciting and challenging time for all young people. But for those with disabilities, including hearing impairments, or those who are dependent on technology such as tracheostomies, moving from children’s to adult health services provides an additional challenge. A team from Alder Hey Children’s hospital in Liverpool, UK, has designed a ‘10 Step Transition Pathway’ to facilitate a smooth transition in to adult healthcare for all young people with disabilities and long-term conditions.
What is transition to adult services?
When children become adults it is normal for them to make decisions for themselves and to lead a more independent life. Children’s health and care needs also change as they grow up. Transition to adult services (transition) is the name given to the process of moving on from children’s to adult services.
“There is a wealth of research evidence documenting the difficulties of transition to adult services and the consequences of poor transition.”
Some young people will have long-term conditions, such as diabetes or epilepsy, and transition will be mainly concerned with moving on to adult health services. Other young people may have learning disabilities or social care needs. Their transition will be more concerned with moving on to adult social or learning disability services. A small number of young people with complex long-term conditions will have support from health, social care and special education. When this happens it is important that these services work together to coordinate the different transitions.
Why do we need transition to adult services?
Transition is important to ensure that services are appropriate for a young person’s needs. Without transition, adults would be nursed on the same wards as babies and children. As people grow older, they are at risk of developing new conditions that are not seen in infancy or childhood and can therefore not be treated in children’s services.
Why is it difficult to ensure a good transition?
Transition to adult services causes significant challenges for young people, their families and healthcare providers.
- Adolescence – the normal physical, emotional and psychological changes that take place as children become teenagers and then adults
- Transfer of care across service and organisational boundaries
- Living with and managing a long-term health condition: for some young people there is the added complexity of living with a disability
There is a wealth of research evidence documenting the difficulties of transition to adult services and the consequences of poor transition [1]. Lack of appropriate preparation and support through transition to adult services is associated with poor patient experience, deterioration in long-term condition management and patients that are lost to follow-up. The need to improve transition is increasingly recognised by care providers, but also by those who commission or inspect healthcare services [2].


Improving transition to adult services in Liverpool Professionals at Alder Hey Children’s Hospital in Liverpool have recognised the importance of transition for many years. Throughout the 1990s, work in Liverpool and other centres across the UK helped to pioneer development of services for young adults with cystic fibrosis: now considered to be an exemplar in transition to adult services [3]. One of the first transitional epilepsy services in the UK was also developed in Liverpool [4]. However, in early 2014 a review of transition within Alder Hey identified significant gaps in transition support for many young people with long-term conditions, particularly where there is no easily identifiable equivalent adult service and where multiple health and social care needs require multiple coordinated transitions.
Development of the 10 Steps Transition Pathway
The team at Alder Hey recognised the need for a unified approach to transition across the hospital and the wider network of healthcare providers, from both adult and children’s services. The team set out to develop a simple, generic transition pathway, based on best practice evidence, flexible enough to be able to support highly complex patients but simple and clear enough to be equally applicable for more simple transitions.
“The 10 Steps Transition Pathway is based on best practice evidence, flexible enough to be able to support highly complex patients but simple and clear enough to be equally applicable for more simple transitions.”
The 10 Steps Transition Pathway was developed using evidence from a detailed literature review together with findings from a series of consultations – including interviews with GPs, focus groups and an online survey – and validated through a one-day workshop including professionals, young people and parents.
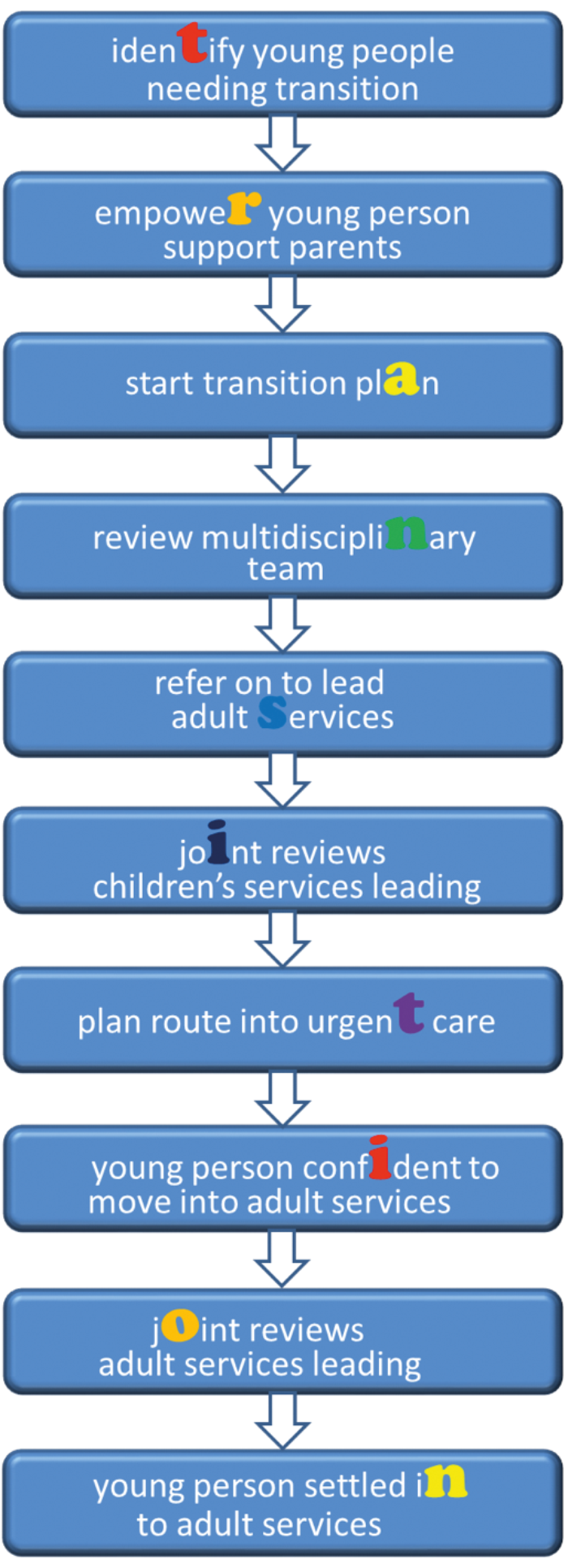
Figure 1. 10 Steps Transition Pathway - Some steps will be started before previous steps are completed.
What is the 10 Steps Transition Pathway?
The 10 Steps Transition Pathway (Figure 1) describes the important steps for a young person, their parents, and professionals, as the young person moves from children’s to adult services and is supported by a growing toolkit (Figure 2) of resources to help make transition smooth, supported and empowered.
The 10 Steps Pathway includes a number of innovative features not found in other transition resources:
- Reviewing the multidisciplinary team and identifying a lead specialty to ensure that transition is coordinated
- Use of the Special Transition Register to actively manage young people for whom timely transition is not possible or appropriate
- Planning the young person’s route into urgent (emergency) care
- Support for young people with long-term conditions diagnosed in transition age
- Scope to incorporate established transition preparation tools such as Ready Steady Go where appropriate [5]
Transition tool kit contents
-
What good looks like: Young person friendly guide for what to expect
-
Empowering the young person and supporting parents
-
Role of Lead Consultant, Keyworker and GP
-
Transition map – specialty-by-specialty transition pathways
-
Special Transition Register – to actively support and monitor young people who remain under children’s services beyond normal transition age.
-
10 Steps Transition Policy for children’s and adult services with auditable standards
-
Competencies for multidisciplinary transition training at universal, core and specialist levels
Figure 2.
Implementing the 10 Steps Transition Pathway
The team at Alder Hey is now implementing the 10 Steps Transition Pathway specialty-by-specialty throughout the hospital. A transition policy including supporting auditable standards, and a staff training package have been developed. Implementation is linked to development of a wider transition framework agreement, including representation from primary care, commissioning, children’s and adult services, health, social care and education across the city.
Implementation is being supported by auditing against the 10 Steps Pathway standards and measuring outcomes including:
- Condition-specific
- Quality of life and participation
- Transition readiness, knowledge and confidence
- DNA rates and loss to follow up
- Young person and family satisfaction
- Incident and near miss reporting
SUMMARY
-
Transition to adult services is necessary to ensure health services remain appropriate for a young person’s needs. However moving from children’s to adult healthcare provision creates significant challenges
-
Smooth safe and effective transition requires a coordinated multidisciplinary approach across children’s and adult services
-
The 10 Steps Transition pathway, developed by the team at Alder Hey Children’s Hospital in Liverpool is flexible enough to support transition of young people with the most complex health and social care needs
-
For more information and access to resources visit www.10stepstransition.org.uk
References
1. Campbell F, Biggs K, Aldiss SK, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev 2016;29:4:CD009794.
2. Care Quality Commission. From the Pond into the Sea. Children’s transition to adult health services. 2014.
www.cqc.org.uk/sites/default/
files/CQC_Transition%20Report.pdf
Last accessed November 2016.
3. Towns SJ, Bell SC. Transition of adolescents with cystic fibrosis from paediatric to adult care. Clin Respir J 2011;5(2):64-75.
4. Rajendran S, Iyer A. Epilepsy: addressing the transition from pediatric to adult care. Adolesc Health Med Ther 2016;27(7):77-87.
5. University Hospital Southampton. Transition to adult care: readty Steady Go.
www.uhs.nhs.uk/Ourservices/
Childhealth/TransitiontoadultcareReadySteadyGo/
Transitiontoadultcare.aspx.
Last accessed November 2016.
Declaration of competing interests: None declared.