Although our operating rooms consume significant resources, some simple changes can have considerable impact in reducing greenhouse gas emissions. Here are 10 such simple things we can do.
Waste is one of the largest contributors to a hospital’s carbon footprint, with the operating room (OR) producing 20-30% of a hospital’s waste [1] and, in a major hospital, contributing to 1165kg of waste per day [2]. Treatment of one patient in the OR is equal to the waste generated by a family of four in one week [1].
Considering this, otolaryngologist-head and neck surgeons (OHNS), and all surgeons for that matter, have a responsibility to reduce the carbon footprint in the OR and promote environmental sustainability. However, in a survey of Canadian OHNS, only 20% strongly believed that the ORs contributed to the climate crisis and, although most believed that environmental sustainability was very important to practise at home, less than half said that it was very important to practise in the operating room [3].
A circular economy is one approach to mitigate OR waste. It is based on the principles of reduce, reuse, and recycle to minimise waste and conserve resources. The patient preparation phase for surgery generates the majority of waste, including opening of consumable supplies, personal protective equipment, and instrument wrapping material [1], such that the principle of reduction has the greatest opportunity for reduction in waste.
"Although most believed that environmental sustainability was very important to practise at home, less than half said that it was very important to practise in the operating room "
There are many opportunities in the OR to reduce and reuse that can be used by OHNS to promote sustainability. Here are 10 changes OHNS can make to reduce their carbon footprint in the OR by following a circular economy approach:
1. Remove single-use table drapes from tonsillectomy/non-sterile procedures.
Rizan and colleagues looked at five common surgical procedures to identify the greatest carbon footprint contributors for these cases. Single-use table drapes were the greatest carbon footprint contributors (11%) of all items used for tonsillectomies, with a mean average carbon footprint of 840g of carbon dioxide equivalents (CO2e) [4]. As these are not sterile procedures, eliminating their use should have no impact on patient care but a substantial impact on the environment. For surgeries that require sterile drapes and setups, consider using reusable sterile drapes and linens, which are more environmentally friendly than single-use disposable drapes.

Single-use drapes from tonsillectomy.
2. Switch to reusable surgical gowns.
Switching from disposable to reusable surgical gowns can reduce a hospital’s carbon footprint significantly by reducing natural energy consumption by 64%, greenhouse gas emissions by 66%, blue water consumption by 83% and solid waste generation by 84% [5]. Additionally, consider eliminating the use of surgical gowns in procedures that do not require gowns (i.e. adenotonsillectomy, endoscopic airway procedures, etc.). The added benefit of this approach was exposed during the pandemic when the supply chain interrupted acquisition of disposable gowns, leaving healthcare workers in institutions without reusable gowns exposed. Additionally, the use of reusable scrub caps is more environmentally friendly, without increased risk of infection, and also has the advantage of allowing personalisation and individuality for the wearer.
"At London Health Sciences Centre, Ontario, 30,600 plastic patient belonging bags are used annually in the OR, producing carbon emissions equivalent to driving approximately 25 times around the earth"
3. Optimise instrument trays.
Waste in ORs from reusable surgical instruments and disposable surgical supplies can be reduced through tray optimisation. Tray optimisation aims to only include surgical instruments and supplies that are necessary and remove instruments and supplies that are rarely or never used. At one hospital, optimising tonsillectomy/adenotonsillectomy trays were projected to decrease annual waste by 1.48 tons and save $830 in waste disposal costs annually [6].
4. Use tap water for laser airway cases.
Laser airway cases require skin and eye protection by placing wet drapes on the patient to appropriately cover these areas and protect against burns. Using tap water instead of sterile water is a cost-effective, safe, and more environmentally-friendly option.
5. Switch to reusable patient belonging bags.
At London Health Sciences Centre, 30,600 plastic patient belonging bags are used annually in the OR, producing carbon emissions equivalent to driving approximately 25 times around the earth. A switch to reusable patient belonging bags, conceivably even where patients bring their own bags, is a more environmentally-friendly option and could save the hospital approximately $3000 annually. Patients can also be encouraged to bring their own water bottles, providing that it aligns with the institution’s infection prevention and control policies.

Plastic patient belonging bags.
6. Reduce plastic packaging of instruments or devices.
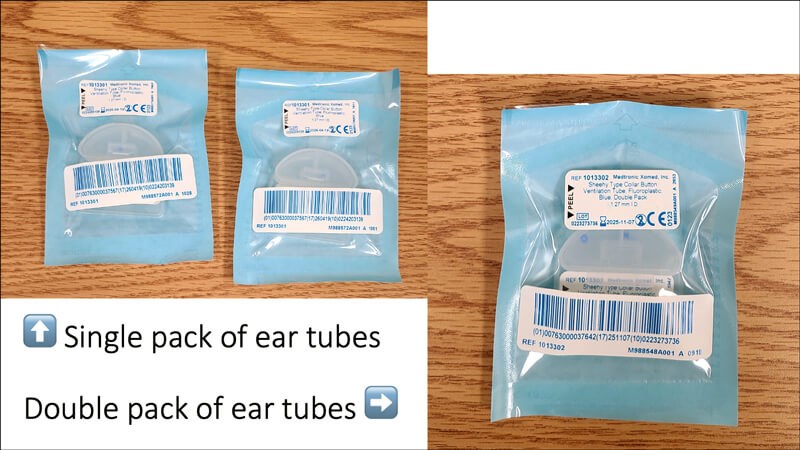
Of all the OR waste produced, 20% is composed of plastic [1] that can take up to 500 years to decompose. Consider reducing single-wrapped instruments and instead package instruments as part of sets on trays. For single-use products, such as ear tubes, procure double packs of ear tubes since, generally, two ear tubes are needed for paediatric patients, and this would reduce plastic packaging waste. For that matter, work with your purchasing team to ensure environmental sustainability is a part of the request for proposal (RFP) process.
7. Reduce the use of single-use devices.
Single-use devices can be reused through reprocessing to reduce waste. Under approved conditions, this practice has not been found to result in increased health risks, as noted by the FDA commissions and the US Government Accounting Office, nor has a higher rate of defective functioning in reprocessed single-use devices been confirmed [1]. Collaborating with industry can promote the practice of reprocessing single-use devices. Or better yet, purchase and/or demand companies to supply reusable devices instead of single-use devices.
8. Use a ‘just in time’ model to prevent overage.
A source of OR waste is overage, which are items that are opened but not used. Using a ‘just in time’ model, ensuring items are available for use but remain unopened unless needed, can help reduce overage and OR costs. Collaboration and open communication amongst surgeons and nurses are needed to make certain that needed supplies are available but opened in an efficient manner and to identify situations which may or may not require certain supplies to be opened.
9. Do procedures under local anaesthesia.
When possible, performing procedures under local anaesthesia avoids the use of volatile gases that contribute to healthcare-associated greenhouse gas emissions and all deleterious effects associated with them. The global warming potential of volatile anaesthetics, desflurane in particular, is significantly higher than for carbon dioxide and methane. Additionally, total intravenous anaesthesia could be considered as an alternative to volatile anaesthetics when general anaesthesia is still required.
10. Advocate and speak up.
Practising environmental sustainability in the OR, and in life, is a moral and public health imperative. Eco-action is the responsibility of all of us. Crucial conversations amongst colleagues and learners and advocating for leadership to prioritise planetary healthcare is paramount.
References
1. Sanabria A, Kowalski LP, Nixon IJ, et al. Considerations for environmentally sustainable head and neck surgical oncology practice. Am J Otolaryngol 2020;41(6):102719.
2. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. The Lancet Planetary Health 2017;1(9):e381-8.
3. Hathi K, Fowler J, Zahabi S, et al. Attitudes and Perceptions of Canadian Otolaryngology‐Head and Neck Surgeons and Residents on Environmental Sustainability. OTO Open 2023;7(1):e40.
4. Rizan C, Lillywhite R, Reed M, Bhutta MF. The carbon footprint of products used in five common surgical operations: identifying contributing products and processes. J R Soc Med 2023;116(6):199-213.
5. Vozzola E, Overcash M, Griffing E. An Environmental Analysis of Reusable and Disposable Surgical Gowns. AORN J 2020;111(3):315-25.
6. Penn E, Yasso SF, Wei JL. Reducing Disposable Equipment Waste for Tonsillectomy and Adenotonsillectomy Cases. Otolaryngol Neck Surg 2012;147(4):615-8.












