After uvulopalatoplasty, the tendency is to focus on the tongue base as the next anatomical area to address in the management of snoring and sleep-disordered breathing. In this article, Glen Burgess describes the technique of tongue channelling, to reduce the size of the anterior tongue.
Airway obstruction from posterior collapse of the tongue has been implicated in the aetiology of sleep disordered breathing in many patients. Until recently treatment of this condition has been problematic. Surgical options have been limited, most complicated by significant morbidity and potential complications.
Treatment for many patients has been limited to dental devices or positive pressure masks. Often these treatments are not well tolerated or have limited beneficial effect. An effective, well tolerated means of reducing airway obstruction from tongue base collapse during sleep has been elusive.
Reduction of the size of the tongue using Coblation® (Arthrocare/ Smith and Nephew, Frenchs Forest, NSW, Australia) was first reported by Zhang [1]. He described using a plasma wand to create carefully placed submucosal channels in the musculature of the tongue, to produce a reduction in total lingual size and hence reduced tongue collapse into the upper airway.
Plasma wand channelling of the tongue has been found to be an effective, safe and tolerable technique to create a reduction in the size of the tongue. This has been effective in producing improved upper airway patency during sleep and the ability to reduce the size of the tongue in other situations where desirable.
Patient selection
- Most patients selected for tongue reduction surgery have significant sleep disordered breathing, as noted on polysomnogram (PSG), and / or troublesome snoring.
- Patients generally present with a history of poor tolerance or lack of success with a continuous positive airways pressure (CPAP) mask and / or mandibular advancement splint.
- A pattern of supine-predominant sleep apnoea is often seen on PSG.
- Clinically, relative macroglossia is often seen with a Freidman Class II or III oral examination [4], combined with significant tongue base collapse upon endoscopic evaluation.
- Clinical evaluation of tongue base collapse is via a nasendoscope passed transnasally and placed in the oropharynx to gauge the site and pattern of collapse. Most patients will have a reduced airway circumference at the level of the tongue base when compared to normal patients.
A complete upper airway examination is performed with careful evaluation of the palate, pharynx and larynx, noting palatine tonsil size, any lateral pharyngeal collapse and presence or absence of lingual tonsils. We perform a series of maximal inhalations and exhalations through the nose and then mouth to assess the airway in various stages of relaxation.
No randomised trials have yet been performed to gauge the reliability of assessment of airway collapse at the tongue base [2], and most surgeons have their own assessment techniques. We have found that if on maximal exhalation mostly lateral pharyngeal collapse is seen, surgical correction of the tongue base should not considered as first line therapy. In the author’s experience, such lateral collapse is mostly due to an excess of weight in the neck. In conditions where both tongue base and lateral collapse occur, treatment needs to be carefully considered and emphasis placed on the importance of weight loss.
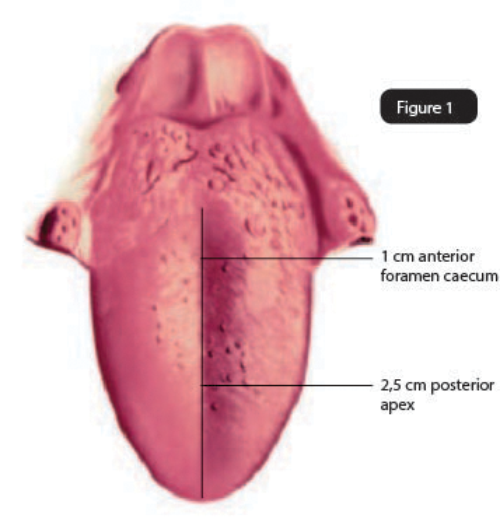
Figure 1: Dorsal topographic anatomy of the tongue.
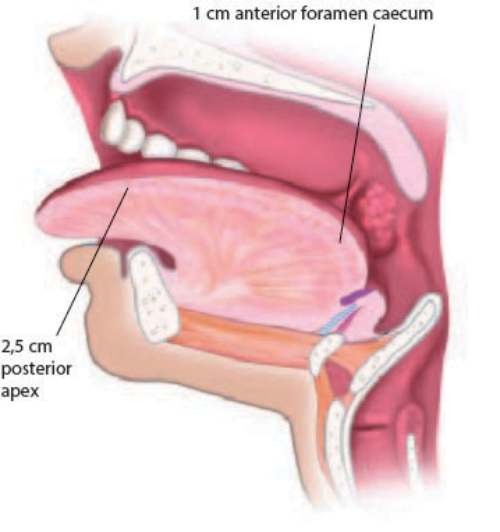
Figure 2a: Lateral view of tongue anatomy.
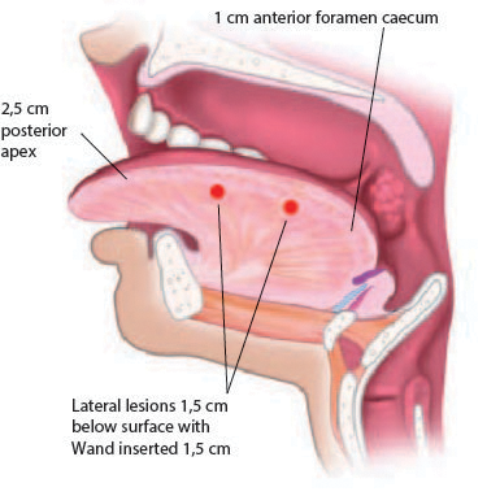
Figure 2b: Diagram of lateral channel positions.
Surgery
Tongue channelling is performed to maximise size reduction and minimise morbidity to the tongue. Channels are placed in the midline and laterally to avoid the lingual neurovascular bundles. Zhang [1] has performed an elegant series of dissections that describe the lingual neurovascular unit and its travel through the tongue from deep and lateral posteriorly to superficial and medial anteriorly. Patients are counselled preoperatively regarding the possibility of damage to these structures. In the author’s experience of over 350 procedures no damage to the lingual or hypoglossal nerves has occurred, nor any significant vascular injury.
Technique
Under general anaesthetic other procedures are initially performed as required (palatine tonsillectomy, palatoplasty, lingual tonsillectomy), then a bite block and lip guard is placed. The tongue is held between fingers in surgical gauze and drawn forward. The circumvallate papillae are identified and the first channel is placed 1cm anterior to the midline papilla. The control box is set to coblation 5 / coagulation 2 and the probe placed into the tongue to the black indicator line (Fig 3). Coblation channelling is then performed for 15 seconds per channel. Further channels are placed at 1cm intervals in the midline until 2.5cm from the tip (Fig 4). Channels are then placed laterally at 1cm intervals along the junction of the keratinised and non-keratinised epithelium until 2.5cm from the tip (Fig 2a, 2b). In tongues with significant lateral width, further channels can be placed midway between the midline and lateral margins of the tongue posteriorly.

Figure 3: Patient positioning and placing the first dorsal channel.

Figure 4: Further dorsal channels.
Postoperative swelling can occur after channelling and is usually able to be managed conservatively. In our experience, problems are rare. We have had two cases of significant swelling, both after more than 20 channels were performed in each tongue; one case required intubation after late swelling at three days postoperatively, and the other settled spontaneously.
Haemorrhage during the procedure is uncommon and if it occurs can generally be managed with bipolar cautery into the channel (using the setting on the wand) and pressure. Rarely a suture through the dorsum of the tongue perpendicular to the channel is required for haemostasis.
In the immediate postoperative period patients are managed with pulse oximety monitoring and general observations. A high dependency unit (HDU) admission can be made for patients with severe sleep apnoea or anaesthetic concerns. Significant postoperative pain from channelling is uncommon. Steroids can be given if swelling is suspected and local treatments with ice and mouth washes are routinely prescribed. All patients are generally discharged after the first night and followed up routinely.
At repeat endoscopy at eight weeks, significant opening of the retrolingual airway and less collapse is routinely seen. Repeat sleep studies are performed at 12 or 16 weeks post operatively. Improvement in the patient’s sleep apnoea continues for many months, and most patients report better sleep at six and 12 months than at three months postoperatively. It is our feeling that after the initial plasma wand dissolution of the tongue is performed – each channel will dissolve approximately eight cubic millimeters of tongue and there may be 20 channels performed – there will be some swelling which will resolve within seven days. There is then a period of collagen formation and cross-linking within each channel which further facilitates tongue size reduction and provides some extra fibrosis within each channel.
We have achieved very significant improvements in the quality of sleep for the majority of our patients and seen very pleasing improvements in apnoea-hypopnoea scores and respiratory disturbance indices in most.
A recent trial of surgery including tongue channelling [3] has confirmed our clinical impressions and results. Further trials are underway to establish selection criteria and individual procedure outcomes. Plasma wand radiofrequency tongue channelling has also been useful to reduce macroglossia in Down’s syndrome and Beckwith-Wiedermann patients where excessive tongue size can give rise to obstructive sleep apnoea and difficulty with mouth closing and drooling.
Our experience using the plasma wand for treatment of supine related obstructive sleep apnoea and reduction of macroglossia has been positive, both subjectively and objectively, with this technique giving us the ability to produce a reliable reduction in tongue size and airway collapse with minimal morbidity and satisfactory outcomes.
References
1. Zhang Q, Song W, She C, et al. Coblation-assisting uvulopalatopharyngoplasty combining coblation-channeling of the tongue for patients with severe OSAHS. J Clin Otorhinolaryngol Head Neck Surg 2012;26:114–7.
2. Woodson BT. Diagnosing the correct site of obstruction in newly diagnosed obstructive sleep apnea. AMA Otolaryngol Head Neck Surg 2014;140(6):565-7.
3. MacKay SG, Carney AS, Woods C, et al. Modified uvulopalatopharyngoplasty and coblation channeling of the tongue for obstructive sleep apnea: a multi-centre australian trial. J Clinical Sleep Medicine 2013;9(2):117-24.
4. Friedman M, Ibrahim H , and Joseph N J. Staging of Obstructive Sleep Apnea/Hypopnea Syndrome: A Guide to Appropriate Treatment.
The Laryngoscope 2004;114(3):454-9.
Declaration of competing interests: Dr Burgess has been employed as a trainer and lecturer by Arthrocare Australasia in running educational programmes for the company.