Landmark Paper: Thomsen J, Bretlau P, Tos M, Johnsen NJ. Ménière’s disease: endolymphatic sac decompression compared with sham (placebo) decompression. Ann N Y Acad Sci 1981;374:820-30.
Of all of the chapters in the Landmark Papers book, the chapter that discussed Thomsen’s paper on endolymphatic sac surgery has proved to be the most popular. Walter Kutz provides his critique of what is a fascinating study on the surgical treatment of Ménière’s disease.
Ménière’s disease is a debilitating disorder presenting with unilateral fluctuating hearing loss, tinnitus, and unpredictable episodes of severe vertigo that lasts for hours. To create more confusion, the exact cause of Ménière’s disease is unknown. Histologic studies of temporal bones in patients with Ménière’s disease show dilation of the scala media in the cochlea, suggesting the symptoms of Ménière’s disease are caused by increased endolymph pressure.
This increased pressure may cause rupture of the inner ear membranes and allow mixing of the endolymph and perilymph, resulting in vertigo and hearing loss.
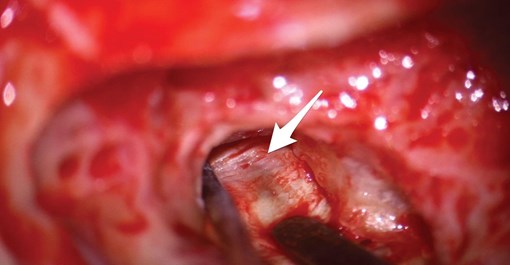
A mastoidectomy has been performed on the left ear.
The bone over the posterior fossa dura and endolymphatic sac
(arrow) has been decompressed.
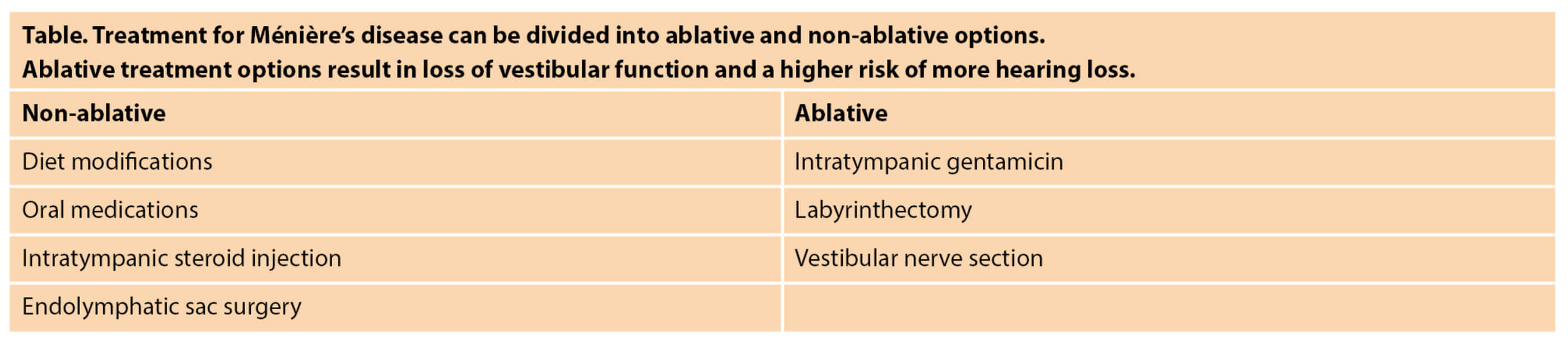
Standard treatment options to control Ménière’s symptoms include a low salt diet, diuretics, betahistine, intratympanic steroid or gentamicin injections, endolymphatic sac decompression with or without shunt placement, labyrinthectomy, or vestibular nerve section. Treatment options can be classified as ablative or non-ablative (table). Ablative treatment options, such as intratympanic gentamicin, labyrinthectomy, and vestibular nerve section, result in loss of vestibular function in the treated ear.
“Studies have shown that decompressing the sac is as effective as placing a shunt, with less chance of permanent hearing loss or spinal fluid leak”
Ablative therapies may lead to problems with chronic imbalance and more hearing loss. Non-ablative treatments spare vestibular function and include diuretics, betahistine, intratympanic steroids, and endolymphatic sac surgery. I typically start treatment with a low salt diet with or without a diuretic. If the patient continues to have episodes of vertigo, betahistine (not FDA approved) and intratympanic steroid injections are offered. If these treatment options do not adequately control vertigo, endolymphatic sac decompression surgery is considered.
“Portman described the first endolymphatic sac surgery in 1927, which would become a standard procedure for the treatment of Ménière’s disease”
Endolymphatic sac decompression surgery is a safe day surgery procedure that takes about an hour. A small incision is created behind the ear, the mastoid bone is removed with an otologic drill, and the bone over the endolymphatic sac is removed. Traditionally, a shunt is placed in the endolymphatic sac, but studies have shown that decompressing the sac is as effective as placing a shunt with less chance of permanent hearing loss or spinal fluid leak [1].
Portman described the first endolymphatic sac surgery in 1927, which would become a standard procedure for the treatment of Ménière’s disease. However, Thomsen had doubts about the efficacy of the endolymphatic shunt procedure and published a randomised sham study in 1981. Thomsen showed both endolymphatic sac decompression and mastoidectomy alone improved dizziness and vertigo symptoms in patients, and endolymphatic sac surgery was not beneficial over a mastoidectomy. The authors concluded the improvement of symptoms after endolymphatic sac surgery was a placebo effect.
Implications for practice and research
Based on this publication, some surgeons have abandoned the procedures; however, the paper has been subject to controversy and criticism. Methodology concerns include a small number of patients (15 subjects in each group). Also, five patients had bilateral Ménière’s disease, and it is possible persistent symptoms after intervention could be from the contralateral ear. There was a significant difference in dizziness and vertigo control favouring the patients who underwent an endolymphatic decompression surgery over the placebo groups (p<0.05). However, the authors report that this difference is ‘slightly significant’ and was no longer present when two placebo patients were removed from the analysis. The authors also state the hearing results were not different between the groups, but they do not provide any audiologic data to support this statement.
“The authors concluded the improvement of symptoms after endolymphatic sac surgery was a placebo effect”
Subsequent studies have refuted the conclusion by Thomsen that endolymphatic sac surgery is not superior to sham surgery. Welling reanalysed the data and concluded that the patients who underwent endolymphatic sac surgery significantly improved in all categories except subjective hearing improvement compared to the placebo group [3]. Pillsbury performed an alternative analysis that showed endolymphatic sac decompression resulted in better dizziness and vertigo control when compared to the placebo group [4].
So how does endolymphatic sac decompression surgery fit into the management of Ménière’s disease? If symptom control with less invasive treatments such as low salt diet, diuretics, betahistine, and intratympanic steroid injections fail, endolymphatic sac decompression surgery offers another low-risk, non-ablative treatment option for Ménière’s disease.
References
1. Brinson GM, Chen DA, Arriaga MA. Endolymphatic mastoid shunt versus endolymphatic sac decompression for Ménière’s disease. Otolaryngol Head Neck Surg 2007;136(3):415-21.
2. Thomsen J, Bretlau P, Tos M, Johnsen NJ. Ménière’s disease: endolymphatic sac decompression compared with sham (placebo) decompression. Ann N Y Acad Sci 1981;374:820-30.
3. Welling DB, Nagaraja HN. Endolymphatic mastoid shunt: a reevaluation of efficacy. Otolaryngol Head Neck Surg 2000;122(3):340-5.
4. Pillsbury HC 3rd, Arenberg IK, Ferraro J, Ackley RS. Endolymphatic sac surgery. The Danish sham surgery study: an alternative analysis. Otolaryngol Clin North Am 1983;16(1):123-7.