Airway stenosis has been an enormous challenge to laryngologists since the dawn of the sub-specialty. Careful evaluation is essential, as this will determine the best treatment. We hear more from one of the UK’s leading airway centres.
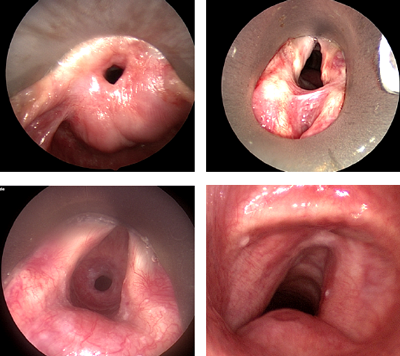
Until the advent of antibiotics in the first half of the twentieth century, infections such as diphtheria, syphilis and tuberculosis were the main cause of laryngotracheal stenosis. However, following the introduction of the ‘Intensive Care Unit’ (ICU), prolonged intubation now accounts for the majority of these cases (Table 1). Laryngotracheal stenosis (Figure 1) can affect all age groups although the pathophysiology, management and long-term results vary between adult and paediatric patients.
In children 95% of stenoses are post-intubation with the majority of others being congenital. The anatomical site is most commonly the subglottis. In adults about 50% are due to ICU ventilation with the other causes being vasculitis, idiopathic, trauma, mucous membrane pemphigoid and sarcoidosis. In adults the site can be anywhere from the supraglottis to the bronchi.
Figure 1. Laryngotracheal stenosis. A) Supraglottic; B) glottic; C) subglottic; D) tracheal.
Assessment and grading of airway stenosis
The larynx and the tracheobronchial tree form the conduit through which respiratory gases pass and secretions are expectorated, between the lungs and the external environment. The larynx is involved in three main functions: airway protection during swallowing, breathing and phonation. Assessment of the stenosed airway should consider these functions, and the impact on them of any proposed treatments.
The patient history will often lead to the cause of the airway compromise, especially if there are coexisting medical problems such as vasculitis or sarcoidosis. The patient should be questioned about exercise limitations, voice and swallowing problems. Subjective and objective measurement tools will be helpful here. One should listen for the noises of breathing at rest and during exertion. Observe for chest recession and the over use of accessory respiratory muscles. Flexible nasal endoscopy is vital to quantify and document cord movement and to look for evidence of an impaired swallow and laryngopharyngeal reflux. Often the nature of the airway problem will be evident. Flexible endoscopy should also be carried out via the tracheostomy (if present) to look for secondary airway problems. Obesity and aspiration are strong contra-indications to airway surgery and should be investigated and managed.
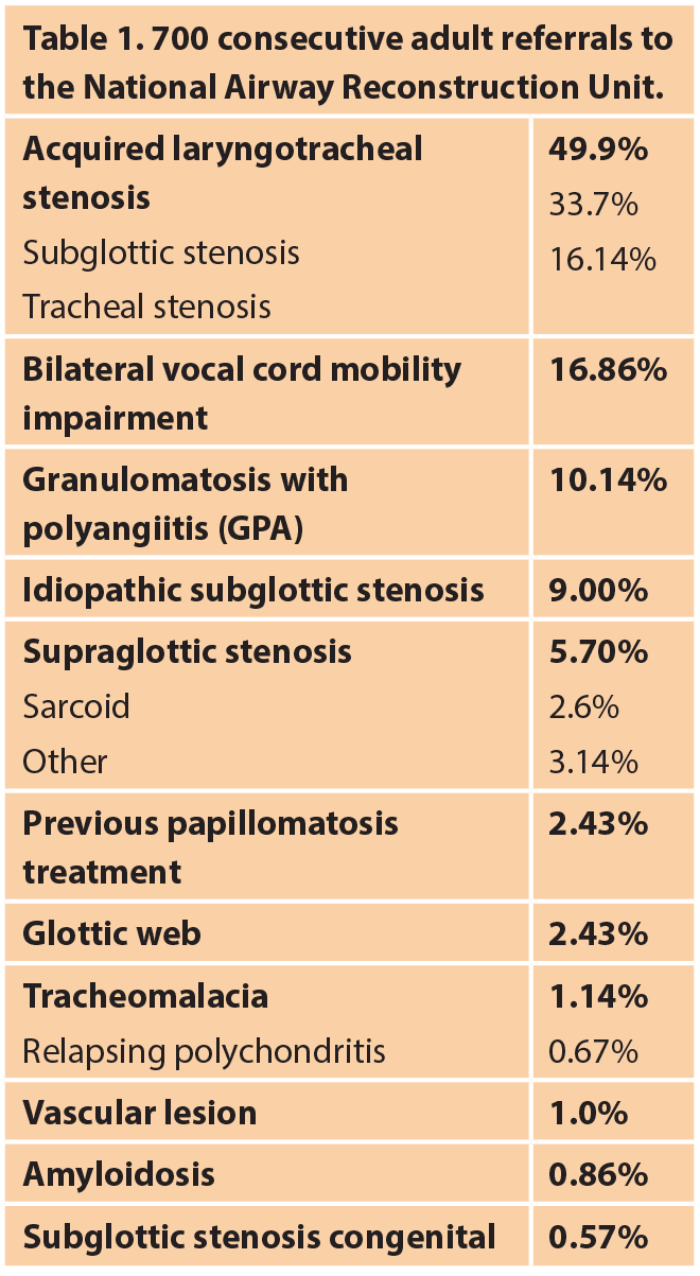
Flow volume loops can aid the diagnosis and differentiate between upper or lower respiratory tract obstruction as well as restrictive lung diseases (Figure 2).
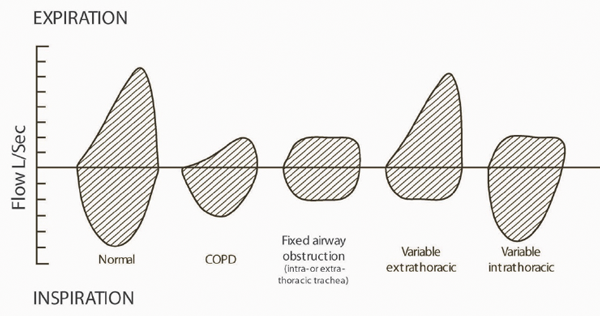
Figure 2. Different patterns of flow volume loops in airway stenosis.
Computed tomography (CT) is the imaging method of choice to help establish the dimensions of the trachea and stenosis, however, in short segment stenosis the axial cuts may miss the narrowest part of the airway and underestimate the severity of the stenosis.
Endoscopic evaluation under general anaesthetic remains the most valuable tool in the assessment of laryngotracheal stenosis. It allows the accurate evaluation of the site, degree and length of the stenosis [1]. The degree of the stenosis can be graded according to the Myer-Cotton system [2] (Figure 3) and provides a good stratification tool. In paediatric patients the airway can also be sized based on the largest endotracheal tube that can safely be passed into the subglottis. Endoscopic evaluation should include instrumentation of the arytenoids to exclude joint ankylosis or scar fixation, exclude laryngeal clefts and assess the trachea and bronchi. In the child, dynamic airway collapse is assessed under general anaesthetic with spontaneous breathing, however, in the adult flexible bronchoscopy under sedation is required.
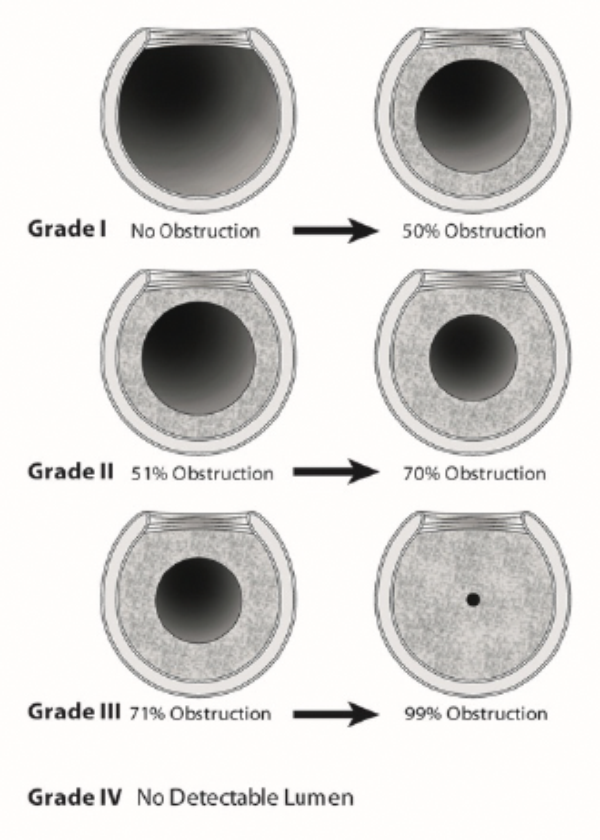
Figure 3. Myer-Cotton classification of airway stenosis.
Paediatric laryngotracheal stenosis
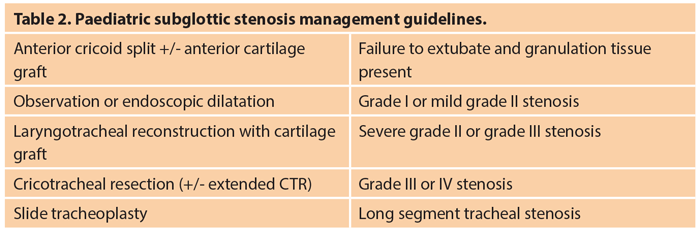
Only about 5% of cases of paediatric subglottic stenosis are congenital. The remainder are acquired and related to prolonged neonatal intubation especially in preterm babies, and those undergoing multiple surgical procedures to correct congenital cardiovascular anomalies. Endoscopic management using balloon dilatation following steroid injection and ‘cold steel’ radial cuts may succeed in mild early cases with web-like short segment stenosis. Open surgical approaches are often applied to severe grade II stenosis and above. The current most common approach is laryngotracheal reconstruction (LTR) using rib cartilage graft to expand the subglottis[3]. Partial cricotracheal resection (CTR) [4] and slide tracheoplasty[5] have been gaining in popularity in the last two decades (Table 2).
Congenital laryngeal webs are part of a spectrum of laryngeal atresia and can be thin, thick or associated with a subglottic stenosis. Treatment will vary from placement of laryngeal keels to the use of LTR or CTR techniques.
Adult laryngotracheal stenosis
Post intensive care laryngotracheal stenosis is the leading cause of airway stenosis in adults. Early post intubation injury can be seen in up to half the patients at extubation on the ICU. The percentage of these patients who go on to develop long-term stenosis is significantly smaller and estimated between 1-4%. Risk factors include duration of intubation, high cuff pressure, poor tube sizing, laryngotracheal reflux, patient agitation and infection. However, it is likely that patients with aggressive healing biology self-select for airway stenosis. More research is required to support this hypothesis.
Endoscopic treatment of post intubation laryngotracheal stenosis is often successful. This involves suspension laryngoscopy, supraglottic jet ventilation and a laser deployed through the microscope using a ‘line-of-sight’ technique. A steroid, such as methylprednisolone, is injected into the lesion, radial cuts are made with the carbon dioxide laser and the stenosis is dilated with an airway balloon to a normal diameter. The rate of success is inversely proportional to the time between intubation and surgical intervention and the length of the stenotic segment [6].
Endoscopic techniques do not work where there is thick mature scar, long segment stenosis and where the cartilaginous airway framework has collapsed. These require tracheal or cricotracheal resection. Standard laryngotracheal reconstruction techniques are not an option in adults. Unlike children, cartilage grafts in adults do not reliably survive as primary airway augments, as they undergo avascular necrosis.
Planning is vital when considering a resection in the adult patient as the trachea becomes less elastic with age. Hence, about 4cm of trachea can be resected reliably with tension free anastomosis. Up to 6cm may be resected with a suprahyoid and pulmonary ligament release.
Idiopathic subglottic stenosis is a rare progressive fibro-inflammatory condition affecting European females after puberty. The exact aetiology is poorly understood, however, the histopathological features are of a submucosal pattern of acute and chronic inflammation mixed with fibrosis.
Classically it involves the lower cricoid and first one or two tracheal rings. The ideal treatment modality remains controversial. While some surgeons advocate cricotracheal resection, others treat this condition with repeated endoscopic dilatations.
Inflammatory conditions such as granulomatosis with polyangiitis (GPA), sarcoidosis, amyloidosis, mucous membrane pemphigoid and IgG4 disease can be associated with laryngotracheal stenosis and often require long-term immune suppression treatment. The main stay of surgical treatment is endoscopic dilatations and steroid injections [7].
Acquired bilateral vocal cord mobility impairment
The causes can be categorised as follows:
- Bilateral denervation (thyroid surgery or neck and chest malignancy)
- Cricoarytenoid joint fixation (rheumatoid arthritis or trauma)
- Inter-arytenoid scarring (post intubation)
Bilateral recurrent laryngeal nerve injuries leave the vocal folds in the paramedian position and patients suffer with significant shortness of breath and demonstrate stridor. They often end up with a tracheostomy in the acute situation. Various techniques have been described to manage this problem and these include laser to the posterior vocal fold or arytenoid, and suture lateralisation of the vocal folds. More recently selective reinnervation approaches have been advocated [8]. Fixation of the cricoarytenoid joints can only be managed with destructive laser procedures to the glottis.
Posterior interarytenoid scar rarely responds to endoscopic division alone. Division and post-cricoid mucosal advancement flaps [9] or placement of posterior cricoid cartilage graft are endoscopic approaches that need further evaluation. The well-established approach is laryngofissure and posterior cricoid split with placement of an autologous cartilage graft. The results of airway surgery on the glottis are always a compromise between voice, airway and swallowing. Pre-existing aspiration is a contraindication.
Conclusion
Laryngotracheal stenosis is a rare but debilitating condition which can have a lifelong impact on a patient’s quality of life. Prevention is therefore vital. Appropriate sizing of endotracheal tubes, monitoring cuff pressure and early tracheostomies are simple but effective measures to reduce the incidence of ICU related airway stenosis. Early recognition and treatment of stenosis due to systemic conditions will also improve outcomes.
References
1. Nouraei SA, McPartkin DW, Nouraei SM, et al. Objective sizing of upper airway stenosis: a quantitative endoscopic approach. Laryngoscope 2006;116(1):12-7.
2. Myer CM, O’Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol 1994;103(4 Pt1):319-23.
3. Cotton RT. The problem of pediatric laryngotracheal stenosis: a clinical and experimental study on the efficacy of autogenous cartilaginous grafts placed between the vertically divided halves of the posterior lamina of the cricoid cartilage. Laryngoscope 1991;101(12 Pt 2 S56):1-34.
4. Monnier PF, Lang F, Savary M. Cricotracheal resection for pediatric subglottic stenosis. Int J Pediatr Otorhinolaryngol 1999;49(S1):S283-6.
5. de Alarcon A, Rutter MJ. Cervical slide tracheoplasty. Arch Otolaryngol Head Neck Surg 2012;138(9):812-6.
6. Nouraei SA, Kapoor KV, Nouraei SM, Ghufoor K, Howard DJ, Sandhu GS. Results of endoscopic tracheoplasty for treating tracheostomy-related airway stenosis. Clin Otolaryngol 2007;32(6):471-5.
7. Nouraei SA, Obholzer R, Ind PW, et al. Results of endoscopic surgery and intralesional steroid therapy for airway compromise due to tracheobronchial Wegener’s granulomatosis. Thorax 2008;63(1):49-52.
8. Marina MB, Marie JP, Birchall MA. Laryngeal reinnervation for bilateral vocal fold paralysis. Curr Opin Otolaryngol Head Neck Surg 2011;19(6):434-8.
9. Atallah I, Mk M, Al Omari A, Righini CA, Castellanos PF. Cricoarytenoid Joint Ankylosis: Classification and Transoral Laser Microsurgical Treatment. J Voice 2018.