Technology is moving our speciality forward very rapidly in all domains, but none more so than in rhinology. David Whitehead looks at current and future trends.
How will a surgeon justify their position in a team where artificial intelligence (AI) and machines outperform humans? Is this fantasy or our future reality? We know that artificial neural networks currently surpass humans in video games, object recognition, voice recognition, art imitation, website modification and predictions [1].
Some areas of medicine lack large, high-quality datasets with which to train the AI algorithms but in other areas, such as radiology, data is being used to train sophisticated algorithms that can outperform the majority of radiologists [2]. In the sphere of rhinology, with enough high-quality data, it is likely that AI systems will encroach on decision-making and will outperform even the experts. In doing so, this will challenge dogmas and open up new areas of research and treatment.
“In the sphere of rhinology, with enough high-quality data, it is likely that AI systems will encroach on decision-making and will outperform even the experts”
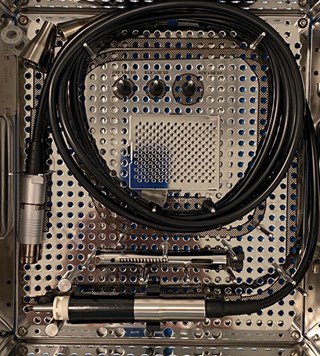
Ultrasonic piezo rhinoplasty set.

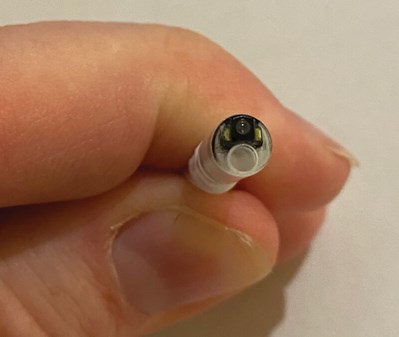
ClariFix intranasal cryotherapy device.

NUVIS disposable rigid endoscope with integrated illumination.
If AI is going to impact on clinical decisions, what should we expect in terms of equipment in the next few years? COVID-19 has seen an acceleration in the use of disposable single-use instruments which have many benefits; it is likely that this trend will continue with disposable ‘chip on tip’ endoscopes [3]. Current systems can be easily integrated into workflows, allowing for storage of images and videos onto central image-storing servers whilst also allowing live transmission of remote endoscopic images using Microsoft Teams, Zoom or Proximie. This has already provided substantial benefits in lowering the risk of exposure to COVID for our juniors but has also allowed us to provide retrospective opinions on examinations performed earlier or offsite.
As the AI and hardware systems develop, everything the surgeon does will be recorded automatically. All images and videos will be classified with automated anatomical identification. The position of the scope and hand movements, as well as the surgeon’s cognitive bias will be calculated. Human capability will be augmented through brain computer interfacing of navigated endoscopic sinus surgery systems.

AMBU disposable flexible naso-endoscope attached to
AMBU aView 2 monitor and streamed live across the internet.
Close up of disposable camera head on Ambu disposable endoscope.
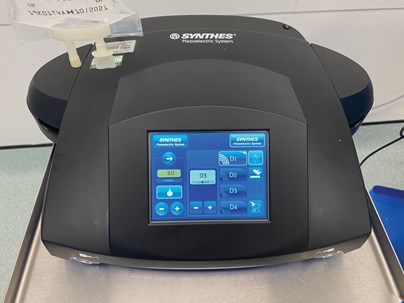
Ultrasonic rhinoplasty controller.
As in all areas of medicine, new therapeutic options are emerging: vasomotor rhinitis is a very challenging condition to treat, and cryosurgery to postganglionic fibres of the pterygopalatine ganglion appears promising (I was the first in the world, outside of North America to use ClariFix) for those with recalcitrant chronic rhinitis. This will help patients who find no benefit from current medical treatments.
Further technological advancements and repurposing may lead to more sinus surgery being performed on the awake patient. Outpatient-based sinus surgery is more technically challenging for the surgeon but is already a reality.
“Human capability will be augmented through brain computer interfacing of navigated endoscopic sinus surgery systems”
Functional rhinoplasty has also seen technological advancement. Three-dimensional surface imaging of patients pre and postoperatively using stereophotogrammetry is traditionally expensive and cumbersome. But smartphone videos can now make an accurate 3D model of a patient’s face, and the iPhone’s TruDepth camera can now reconstruct a virtual high-resolution version of the face. The recent introduction of a LiDAR (Light Detection and Ranging) sensor on the new iPhone will make this process faster and more accurate.
“The precision that is achievable with piezo would be hard to replicate even with a fine rasp”
Ultrasonic or piezoelectric rhinoplasty was first reported by Robiony [4] and popularised by Olivier Gerbault [5] in Paris, France. It allows for more accurate osteotomies and sculpting of the nasal and maxillary bones whilst preventing injury to soft tissue such as cartilage. The precision that is achievable with piezo would be hard to replicate even with a fine rasp. In some cases, osteotomies can be avoided completely. The device and ultrasonic inserts are expensive but the precision and consistency achievable is superb. For these reasons, it is likely to gain in popularity.
The real question is not whether machines think but whether men do [6].
References
1. Yim J, Chopra R, Spitz T, et al. Predicting conversion to wet age-related macular degeneration using deep learning. Nat Med 2020;26(6):892-9.
2. Rodriguez-Ruiz A, Lång K, Gubern-Merida A, et al. Stand-Alone Artificial Intelligence for Breast Cancer Detection in Mammography: Comparison With 101 Radiologists. J Natl Cancer Inst 2019;111(9):916-22.
3. Ambu single-use ENT rhinolaryngoscopes.
www.ambu.co.uk/endoscopy/
ent-otorhinolaryngology
Last accessed November 2020.
4. Robiony M, Polini F, Costa F, et al. Ultrasound piezoelectric vibrations to perform osteotomies in rhinoplasty. J Oral Maxillofac Surg 2007;65(5):1035-8.
5. Gerbault O, Daniel RK, Kosins AM. The Role of Piezoelectric Instrumentation in Rhinoplasty Surgery. Aesthet Surg J 2016;36(1):21-34.
6. Skinner BF. Contingencies of Reinforcement: A Theoretical Analysis 1969.




