While many patients with chronic rhinosinusitis respond to medical treatment, some do not. The next step for these patients is surgery, but how soon should this be offered? Sooner rather than later seems to be the answer, as Claire Hopkins explains.
Chronic rhinosinusitis (CRS) is a common condition with a prevalence estimated at 11% of UK adults. It has significant impact on quality of life and socio-economic burden. Widely held consensus mandates a trial of maximum medical therapy as the first line of treatment, with surgical intervention reserved only for cases refractory to medical management.
The European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) suggests a number of therapies, including steroid (topical or oral), antibiotics and / or saline irrigation, for at least 12 weeks [1]. Review of the literature regarding the success rates of such regimes suggests that roughly 50% patients seen in secondary care will respond, although some will go on to develop a symptomatic relapse thereafter. Failure of medical therapy or relapse after medical treatment would be considered an indication for surgery.
“Once medical treatment has failed it may be detrimental to continue with repeated courses of unsuccessful treatment.”
However, what constitutes ‘maximum medical therapy’, and for how long this should be continued before ‘failure’ is declared, remains uncertain [2]. There is little in the literature to inform on the optimum timing of surgical intervention beyond that failed three-month time window. As a result, many patients in the UK undergo repeated courses of medical therapy for CRS, and surgical intervention is often considered only after many months or years of symptomatic disease.
Timing of surgical intervention in the UK
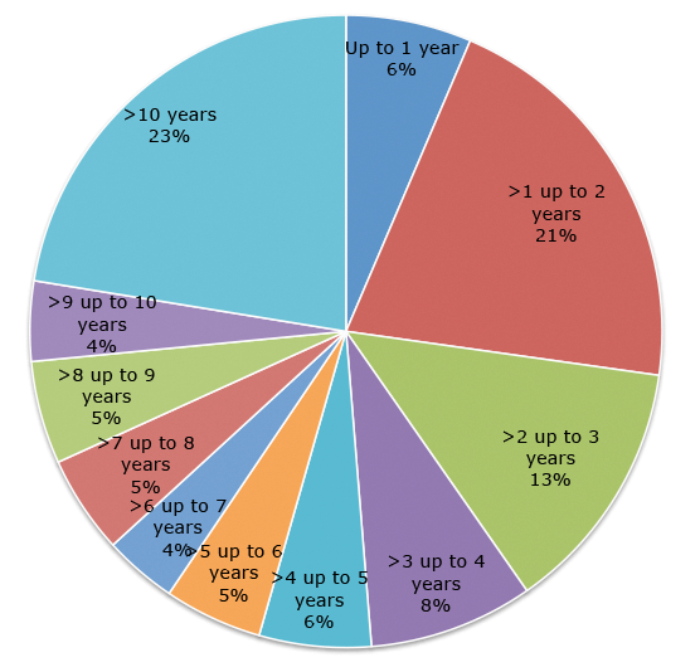
Analysis of UK CPRD data (Figure 1), an electronic dataset that captures all healthcare interactions, suggests that 10% of patients with CRS seen in secondary care were referred within two years of their first recorded CRS diagnosis, the remainder at a later stage. The median number of primary care visits prior to referral was 3.7. Each visit was associated on average with the prescription of two different classes of medications, most commonly antibiotics and intranasal corticosteroids. For patients undergoing endoscopic sinus surgery (ESS) in 2012, the median time to surgery from first observed CRS diagnosis was 4.5 years with only one in four patients undergoing surgery within two years.
Figure 1. UK data on time from onset of CRS to first surgical intervention
for patients identified as having endoscopic sinus surgery.
Does a delay in surgery affect outcomes?
There is little evidence in the literature to inform whether this apparent delay in surgical intervention, accompanied by repeated courses of medical treatment, may have a detrimental effect on outcome. Smith et al. [3], in a prospective, non-randomised multi-centred cohort study, offered CRS patients refractory to medical therapy either continued medical management or endoscopic sinus surgery according to patient and surgeon preference. While this inherently introduces bias to the study, this design provides an appropriate reflection on the decision-making process that patients and surgeons face at the time of failed medical therapy. Thirty-four percent of the medical management arm did not improve and further worsened within three months of entering the study, and then crossed over into the surgical treatment arm. While these patients experienced significant improvements in patient rated symptom scores, at 12 months’ follow-up they had failed to achieve the same level of symptomatic improvement as the cohort who had undergone surgery ab initio.
Although this non-responder group may simply reflect more recalcitrant disease, perhaps delaying surgical intervention may have adversely affected outcome in refractory patients. Again, little is known of the natural history of CRS, but it is possible that untreated chronic sinusitis is a progressive disease and with time patients develop irreversible changes within the sinus mucosa, or that the treatment itself has detrimental effects.
In order to evaluate this further, data from both the UK audit of surgery for CRS and CPRD data were analysed [4, 5]. Patients were classified according to duration of CRS until their first surgical intervention for CRS. Three cohorts of patients were defined: early cohort – less than 12 months; mid cohort – 12-60 months; and late cohort – more than 60 months of symptoms (Figure 2). In the UK Audit 1493 patients having primary surgery were identified; 11.5% in the early, group, 50.2% in the mid group and 38.2% in the late group. Patients in the early group had not only a greater percentage improvement in their symptoms, but the improvement was better maintained over five years. At five years there was a significantly higher proportion of patients in the early group maintaining a clinically significant improvement over baseline (71.5%) than in either the mid (57.3%) or late (53.0%) groups.
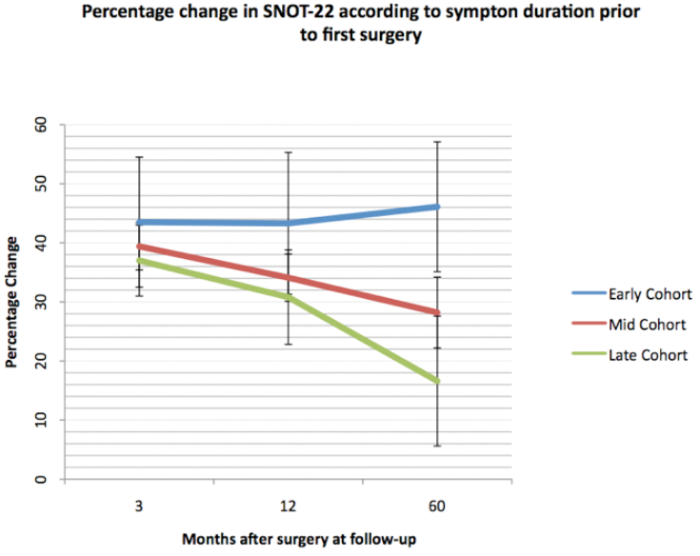
Figure 2. Percentage change in SNOT22 scores after surgery, by timing of first surgical intervention.
Using healthcare interactions as a proxy for symptomatic improvement in CPRD (assuming that higher frequency of healthcare visits and prescription medications reflect a poorer outcome from surgery), a similar pattern is found. Patients having early surgery see their GP less frequently and receive fewer prescription medications each year after surgery than the mid or late cohorts (Figure 3). These results have been further replicated in a US based electronic dataset.
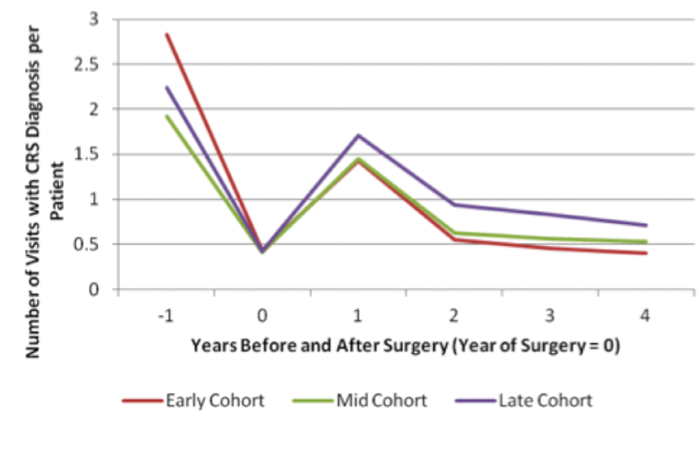
Figure 3. Number of primary care interactions for CRS per annum, by timing of first surgical intervention.
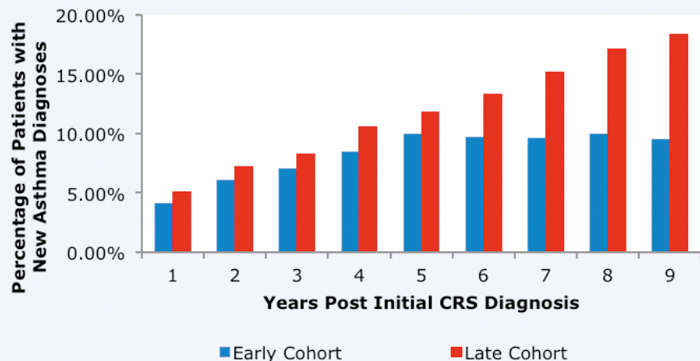
Perhaps of even greater interest to the population as a whole, we also analysed the impact of ESS on the subsequent development of asthma. We have found, using both UK and US datasets, that ESS is associated with a reduction in the incidence of new asthma diagnoses following surgery, and that the reduction is greatest in those having early surgery (Figure 4) [6].
Figure 4. Prevalence of asthma in patients undergoing ESS (patients with asthma prior to onset of CRS have been excluded).
Patients having surgery in year 2 shown in blue, patients where surgery is delayed until year 10 shown in red.
Why might early surgery be associated with improved outcomes?
Theories that ESS improves symptoms by restoring sinus ventilation have recently been challenged, particularly in patients with CRS with polyps, or eosinophilic inflammation where the ostiomeatal complex often remains patent even in the presence of extensive sinus disease. However, the importance of surgery in allowing good access for intranasal corticosteroids and other topical therapies is increasingly recognised.
There is also growing evidence to support an association between recalcitrant disease and a higher inflammatory load [7] – accumulation of biofilms and eosinophilic mucus, mucosal remodelling and the development of osteitic bone are all poor prognostic factors and are likely to develop over time. Earlier intervention may allow more effective treatment of disease before such factors develop. Another emerging concept in CRS is the importance of the microbiome; the healthy sinus is not sterile, but there is a change in the diversity and prevalence of bacteria in the diseased state. It is possible that repeated courses of antibiotics may actually be detrimental by altering the natural microbial biodiversity of the sinuses.
“Early surgical intervention appears to be associated with better long-term outcomes.”
Implications for clinical practice Endoscopic sinus surgery should still be reserved for patients who remain symptomatic despite a reasonable trial of medical therapy. However, once medical treatment has failed it may be detrimental to continue with repeated courses of unsuccessful treatment. A ‘medical merry-go-round’ where patients receive multiple courses of antibiotics and steroids over many years should be avoided. Early surgical intervention appears to be associated with better long-term outcomes and is likely to also be cost-effective. Commissioning pathways in the UK should reflect this to avoid unnecessary delays in referral.
References
1. Fokkens WJ, Lund VJ, Mullol J, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol Suppl 2012;3p preceding table of contents, 1-298.
2. Orlandi RR, Kingdom TT, Hwang PH, et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int Forum Allergy Rhinol 2016;6(S1):S22-S209.
3. Smith KA, Smith TL, Mace JC, Rudmik L. Endoscopic sinus surgery compared to continued medical therapy for patients with refractory chronic rhinosinusitis. Int Forum Allergy Rhinol 2014;4:823-7.
4. Hopkins C AP, Holy C. Does time to surgery impact on outcomes from endoscopic sinus surgery - data from the UK CPRD database. Rhinology 2015;51.
5. Hopkins C, Rimmer J, Lund VJ. Does time to endoscopic sinus surgery impact outcomes in Chronic Rhinosinusitis? Prospective findings from the National Comparative Audit of Surgery for Nasal Polyposis and Chronic Rhinosinusitis. Rhinology 2015;53:10-17.
6. Benninger MS, Sindwani R, Holy CE, Hopkins C. Impact of medically recalcitrant chronic rhinosinusitis on incidence of asthma. Int Forum Allergy Rhinol 2016;6:124-9.
7. Bassiouni A, Naidoo Y, Wormald PJ. When FESS fails: the inflammatory load hypothesis in refractory chronic rhinosinusitis. Laryngoscope 2012;122:460-6.
Declaration of Competing Interests: None declared.