In the second of our series on local skin flaps (see Part 1 here, Part 3 here and Part 4 here), the authors describe more techniques and examples of various skin flaps that trainees should find very interesting.
Rhomboid flap
This remains our ‘workhorse’ flap and is useful over the cheeks, temples and upper neck. It can also be used for smaller areas over the nasal dorsum and lateral nasal subunits. The flap can reconstruct a defect from four directions, providing options for concealment. The defect can remain circumferential in pattern to preserve skin with the rhomboid transposing in without affecting closure (Figures 1-4) [1].
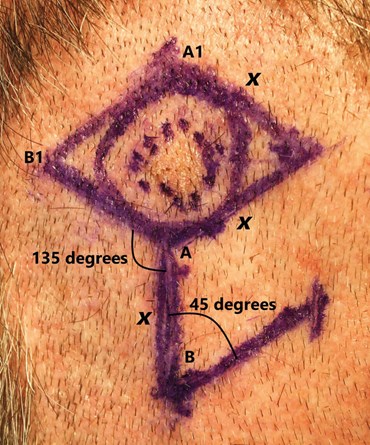
Figure 1. The flap transposes over a 45o angle, with A and B being positioned to the
A1 and B1 points. Uniform defect and flap length measurements (x) permit adequate closure.
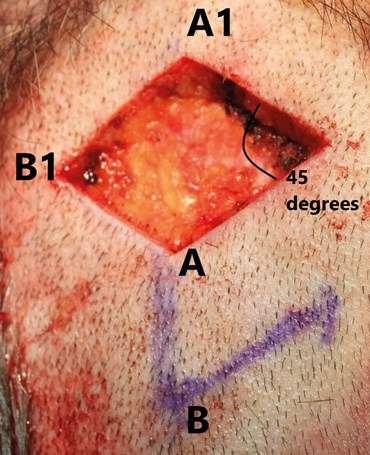
Figure 2. Excision beneath the reticular dermis ensures preservation of the skin’s
blood supply. Flap depth should match that of the defect to ensure aesthetic closure.

Figure 3. Surrounding skin is undermined to close the
secondary defect and is sutured at the flap’s base.
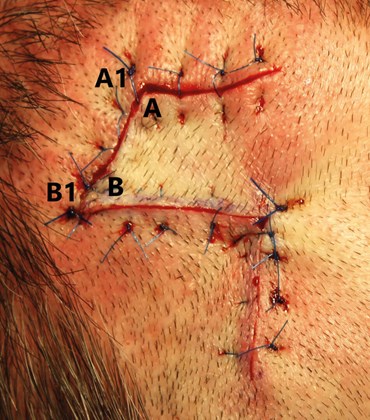
Figure 4. Vertical mattress sutures placed outside of the flap to minimise trauma.
Bilobed flap
We use the Zitelli modification of the original Esser design, as the narrower angles between lobes allow greater skin preservation [2]. This is especially useful in reconstruction on the external nose and can be used across all its subunits as well as where large defects are formed in thinner skin e.g. the supraclavicular fossa.
Tissue adjacent to the lesion on the y-axis must be excised to allow transposition of the base of the first lobe into the primary defect. The shared base of the first and second lobes should be kept as wide as possible to maintain the blood supply to the flap. The skin surrounding the primary defect and first lobe defect may require considerable undermining to achieve a tension-free wound closure, though very little undermining is required to close the second lobe defect due to its narrower width (Figures 1-7).
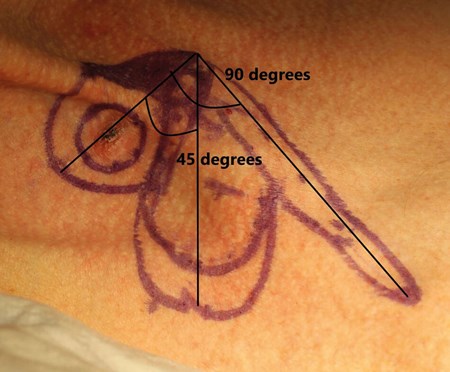
Figure 5. The dimensions of the first lobe are approximately equal to that of the defect,
whereas the second lobe may need to be up to twice as long, though half as wide.
The first and second lobes share a long base to maintain a satisfactory blood
supply and number of perforator vessels.

Figure 6. Excision of an additional triangle of skin adjacent to the defect
is essential to allow unobstructed transposition of the first lobe of the flap.

Figure 7. The defect with the triangle of skin excised. When raised, the lobes of the flap
can appear inadequate for closing their respective defects due to both contracture towards
their base and curling of their edges but redesign is usually unnecessary.
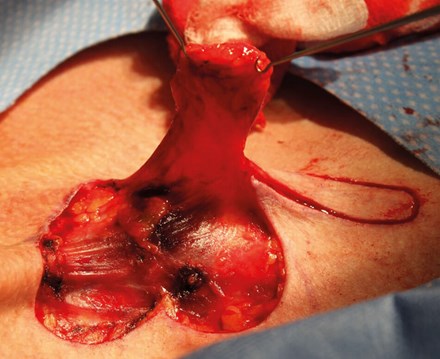
Figure 8. Deeper dissection towards the base will broaden it,
preserving blood supply and facilitating transposition.
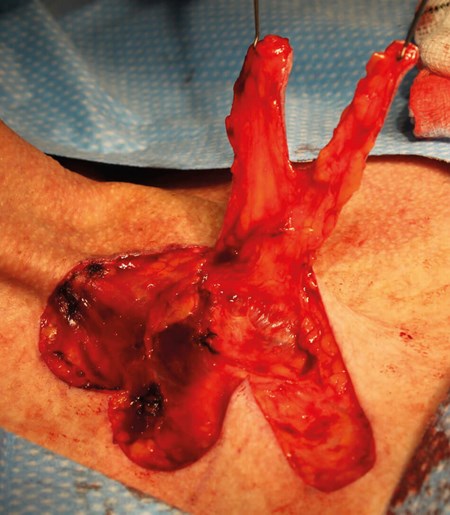
Figure 9. Wider flap bases maintain decent blood supplies to the lobes of the flap.
Gentle handling with skin hooks reduces trauma to the lobes, particularly the small vessels.
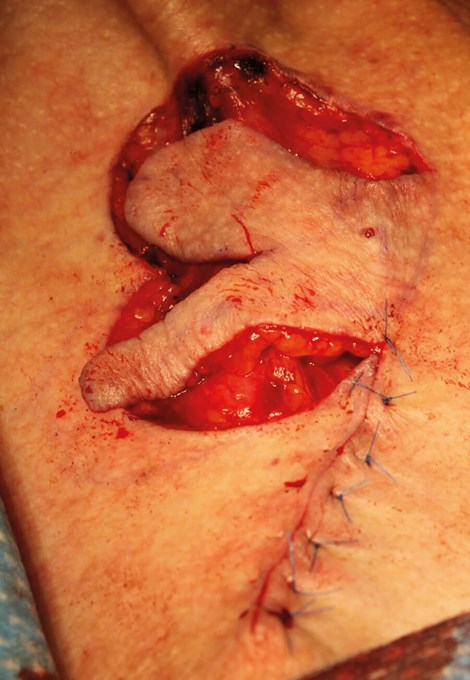
Figure 10. Closure of the second, then first lobe defects facilitates closure of the larger, primary defect.

Figure 11. Completed bilobed flap.
References
1. Quaba AA, Sommerlad BC. ‘A square peg in a round hole’: a modified rhomboid flap and its clinical application. Br J Plast Surg 1987;40(2):163-70.
2. Zitelli JA. The bilobed flap for nasal reconstruction. Arch Dermatol 1989;125(7):957-9






