Bob Carlyon gives us a psychophysical perspective on the hearing benefits that can and cannot be achieved for patients with single-sided deafness with a cochlear implant, and discusses some of the challenges in maximising the effectiveness of the treatment. He also describes the contribution that this group of patients can make towards our understanding of the electrically-stimulated auditory system.
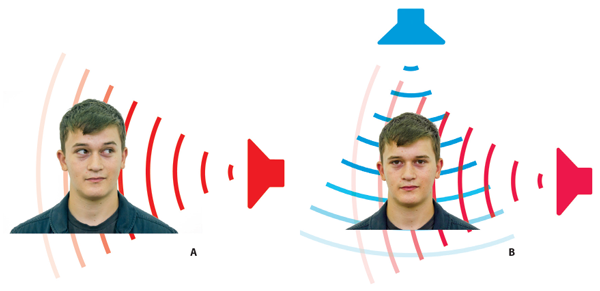
Figure 1: A) A normal-hearing listener is presented with a sound coming from the left. The waveform reaches the right ear later than it reaches the left ear, and, due to the head shadow effect, has a lower intensity at the right than at the left ear. B) One sound, shown in blue, originates from above the listener’s head; the waveform is identical at the two ears; it is inter-aurally correlated. (The same would occur for a sound coming from straight ahead). A fainter sound, coming from his left, interferes with this correlation because its waveform is different at the two ears. The brain can use this decorrelation to understand speech in noisy situations.
What is the best way to treat a patient having a profound hearing loss in one ear and good hearing in the other? Patients with single-sided deafness (SSD) suffer not only from a loss of audibility of sounds coming from their ‘deaf side’, but also from an inability to use binaural hearing to localise sounds and to listen in noisy situations. As shown in Figure 1A, listeners with bilaterally normal hearing use differences in the level and timing of the waveforms reaching the two ears to help them localise sounds.
In addition, when two sounds, such as the voices of competing talkers, come from different locations in space, listeners can use binaural hearing to pick out the talker of interest (Figure 1b). They do so in at least two ways. The simplest is known as the ‘better ear effect’: when the target and masker voices are in different places, the target-to-masker ratio will always be greater at one ear than the other, and listeners can choose which ear to listen to.
Another trick up the brain’s sleeve is illustrated by the situation where a masker is directly above or in front of the listener (Figure 1B), so that the waveforms reaching the two ears are perfectly correlated. When the target voice comes on it reduces this correlation in a way that allows the listener to understand what is being said. Finally, even when the target and masker come from the same location, normal-hearing listeners obtain a ‘binaural summation’ benefit, simply from hearing through two ears rather than one.
In the UK, the most common treatments for single-sided deafness are the CROS aid and the BAHA, which involve routing sound from the ‘deaf side’ to the normal-hearing ear. These solutions restore audibility of sounds on the deaf side, but not the binaural advantages described above and in Figure 1. The only device that does restore some degree of binaural hearing is the cochlear implant (CI). Because of their cost, the NHS does not provide cochlear implants to UK patients with SSD. However, a small number of such patients have been implanted in the UK for the alleviation of tinnitus in the deaf ear, and there is indeed evidence that this treatment is successful [1]. The provision of CIs for SSD patients varies markedly around the world; in some countries, such as Germany and Austria, a CI can be provided as long as it is the best possible treatment for the deaf ear, even if the patient’s other ear is completely healthy. In this short article I will discuss the hearing benefits that can and cannot be achieved with a CI, and discuss some of the challenges in maximising the effectiveness of the treatment. I will also describe the contribution that this group of patients can make towards our understanding of the electrically-stimulated auditory system. The signal processing performed by CIs removes most of the fine timing information present in a sound. Therefore, SSD patients will not be able to localise sounds or extract them from noisy situations using inter-aural differences in timing.
However, they may still be able to localise sounds based on between-ear differences in level (the ‘head shadow’ effect), and can select which of two spatially separated sounds to attend to via the better-ear effect. Indeed, there is evidence that SSD patients can use their CI to help understand speech in presence of a spatially separated masker [1]. The quality of the speech coming from the CI will of course be degraded, and so it comes as no surprise that listeners do not obtain an advantage when the target and masker come from the same location [1, 2]. In addition, when there is just a single speaker close to the deaf ear, we might expect patients to perform better with a CROS aid or BAHA, which route the sound to a normal-hearing ear, compared to a CI where the sound is degraded by the CI processing and by the damaged auditory pathway on the deaf side.
One factor that may limit the potential benefit of a CI is that the electrode arrays produced by most CI companies are not fully inserted along the length of the cochlea (an exception being those manufactured by the MedEl company). As a result, the lowest frequency band that the implants convey – which is typically centred on about 200 Hz – may be conveyed by an electrode whose position in the cochlea corresponds to a much higher frequency. This mismatch can lead to an ‘unfused’ perceptual image, at least at first, and may discourage the patient from using his or her implant. The effective position of each electrode can be obtained either from CT scans or by asking the patient to match the pitches of stimuli presented to the implanted and normal-hearing ear. In a recent study [4] in which patients were implanted with an Advanced Bionics implant, we found that the position of the most apical electrode corresponded to a frequency that ranged between 791 and 967 Hz. The clinician then faces an interesting choice, as illustrated in Figure 2: should one programme the implant as if the other ear were deaf, thereby conveying the full bandwidth of speech, but to mismatched places in the two ears? Or should one omit the lower frequency bands, so that some speech information is lost, but with each frequency band being sent to a cochlear location that matches that in the other ear? This might then be more acceptable to the patient, and improve localisation abilities.
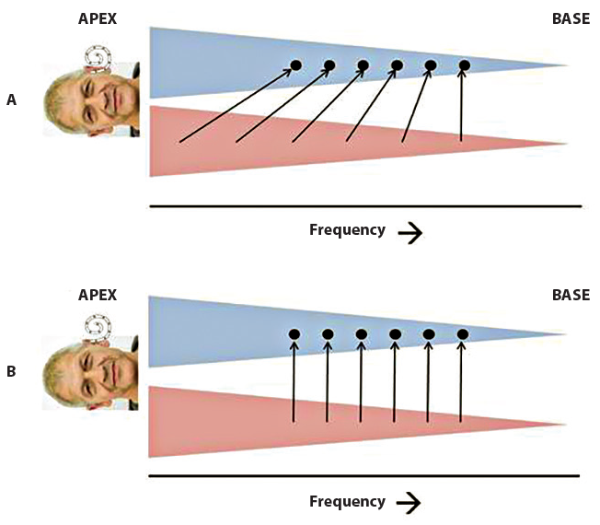
Figure 2: A listener with normal hearing in the right ear and a CI in the left ear, and who has aged badly since Figure 1. The left and right cochleas have been unrolled and are shown by the blue and red triangles, respectively. Part A shows the conventional fitting strategy in which a wide frequency range of sound is compressed onto the range of electrodes in the CI, which do not reach the apex. Part B shows the suggested non-compressed mapping, in which a given frequency will excite analogous portions of the cochlea in both ears.
I think that there is a case for the latter approach, because the head shadow effect is quite weak at low frequencies. The patient is therefore unlikely to miss out on any low-frequency information that is omitted from his or her CI programme, because an only mildly-attenuated copy of that information will be presented to the normal-hearing ear. We have used a compromise between the two approaches with good results,[4] but should stress that the relative merits of the two approaches have not been formally compared.
Finally, SSD patients may allow us to answer the intriguing question of what a cochlear implant actually sounds like. Most people, of course, either have a CI and are deaf, so may forget (or have never experienced) the quality of sound heard through a healthy ear, or do not have a CI and therefore have no experience of what that sounds like. Lazard et al [3] asked patients with some residual low-frequency hearing in one ear to compare various sounds played to that ear to a pulse train presented on an apical electrode of the CI in their other ear. The results were quite variable, but the best match was often to an inharmonic complex tone, that in one case was described as like a boat horn. We have performed a similar experiment with three listeners having normal hearing in their implanted ear; two said that a one third-octave filtered complex tone provided the best match, while a third chose a pure tone.
To summarise, CIs can help SSD patients to localise sounds using inter-aural level cues, and to pick out the voice of one speaker from noisy surroundings using the better-ear effect. These benefits occur even though they do not allow patients to exploit the fine inter-aural timing differences that are accessible to people with normal hearing in both ears. Although I have focussed on the benefits to hearing, it should also be noted that a CI can alleviate tinnitus in the implanted ear. A limitation is that the quality of the auditory information provided by the implant is less than that when sounds are presented to a normal-hearing ear. I have argued that the benefits and acceptance of a CI in SSD may be maximised by using a programme that omits low-frequency information and stimulates regions of the cochlea that are matched to that occurring in the normal-hearing ear. Finally, the cooperation of SSD patients can provide us with unique insights into the percepts experienced by CI patients, and of the fidelity with which the brain processes electrical stimulation of the auditory nerve.
References
1. Arndt S, Aschendorff A, Laszig R, Beck R, Schild C, Kroeger S, Ihorst G, Wesarg T. Comparison of pseudobinaural hearing to real binaural hearing rehabilitation after cochlear implantation in patients with unilateral deafness and tinnitus. Otol Neurotol 2011;32:39-47.
2. Mertens G, Punte AK, De Bodt M, Van de Heyning P. Binaural auditory outcomes in patients with postlingual profound unilateral hearing loss: 3 years after cochlear implantation. Audiol Neuro-Otol 2015;20:67-72.
3. Lazard DS, Marozeau J, McDermott HJ. The sound sensation of apical electric stimulation in cochlear implant recipients with contralateral residual hearing. Plos One 2012;7.
4. Carlyon RP, Macherey O, Frijns JHM, Axon PR, Kalkman RK, Boyle P, Baguley DM, Briggs J, Deeks JM, Briaire JJ, Barreau X, Dauman R. Pitch comparisons between electrical stimulation of a cochlear implant and acoustic stimuli presented to a normal-hearing contralateral ear. Journal of the Association for Research in Otolaryngology 2011;11:625-40.
Declaration of Competing Interests: The author has recently been working as a paid consultant to Advanced Bionics as part of a study of cochlear implants as a treatment for single-sided deafness. He is also in receipt of a research grant from them in respect of an unrelated project.




