Exploring how hearing loss heightens fall risk and how integrated audiologic, vestibular and technological strategies can transform balance care and prevention.
Hearing impairment is one of the most common chronic health conditions worldwide, affecting an estimated 466 million people according to the World Health Organization [1]. Its prevalence increases sharply with age, with nearly two-thirds of adults over the age of 70 experiencing clinically significant hearing loss [2].
While the consequences of hearing loss for communication and social participation are well documented, there is growing recognition of its role as an independent risk factor for balance dysfunction and falls. Falls represent a leading cause of morbidity, mortality and healthcare costs in older adults [3].
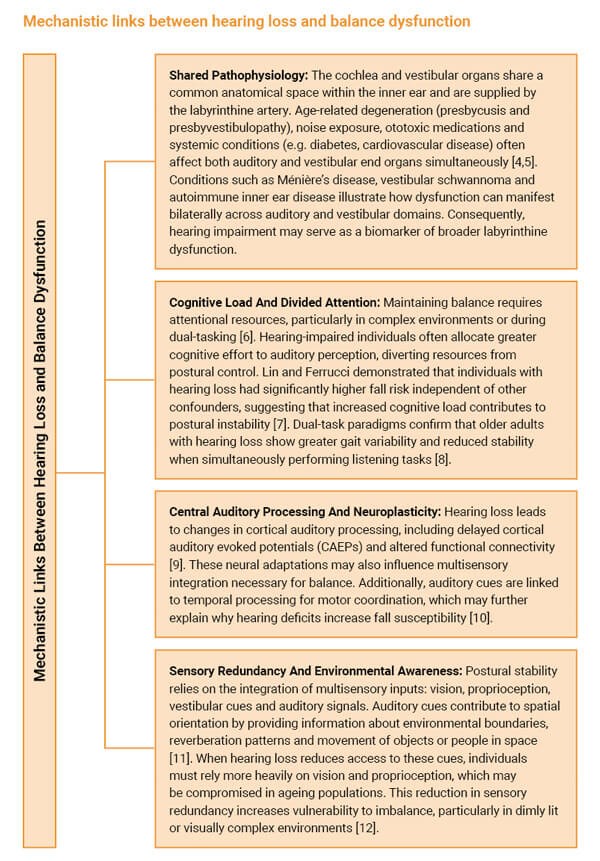
Recent evidence highlights how auditory deficits may impair balance control through multiple pathways, including shared pathophysiology with the vestibular system, reduction in sensory redundancy, increased cognitive load and reduced spatial awareness. Moreover, the integration of balance assessment and fall-prevention strategies into audiologic and otologic practice is emerging as a necessary standard of care. This review expands on prior insights by providing a comprehensive examination of the mechanisms linking hearing loss to balance dysfunction, the epidemiological evidence, clinical assessment strategies, rehabilitation approaches, technological innovations, public health implications and directions for future research.
Epidemiology: linking hearing loss and falls
Several large-scale epidemiological studies have established the association between hearing impairment and fall risk:
- Viljanen et al [13]: In a Finnish longitudinal study, self-reported hearing difficulties predicted increased risk of mobility decline and falls over a 10-year period.
- Lin & Ferrucci [7]: Using NHANES data, they found that every 10 dB increase in hearing loss was associated with a 1.4-fold increase in the odds of reporting falls.
- Agmon et al [14]: Older adults with hearing loss had significantly worse gait and balance performance on standardised tests compared to normal-hearing peers.
- Riska et al [15]: Hearing aid use was associated with reduced fall risk, highlighting the potential mitigating effects of auditory rehabilitation.
Collectively, these findings underscore hearing impairment, not merely as a correlate but as an independent risk factor for balance dysfunction and falls. Importantly, the relationship persists even after controlling for age, vestibular dysfunction and comorbidities.

Clinical assessment strategies
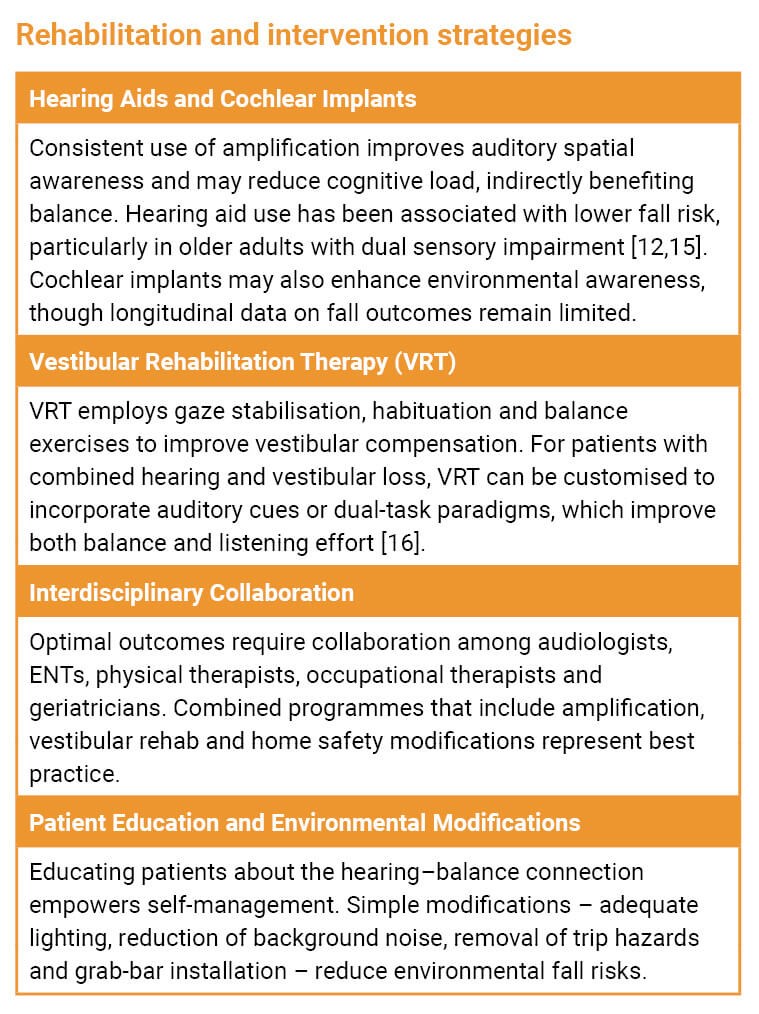
Given the strong evidence linking hearing loss and fall risk, audiologists and otolaryngologists should integrate fall-risk assessment into routine clinical evaluations, especially for older adults. A multidisciplinary framework ensures early identification and intervention.
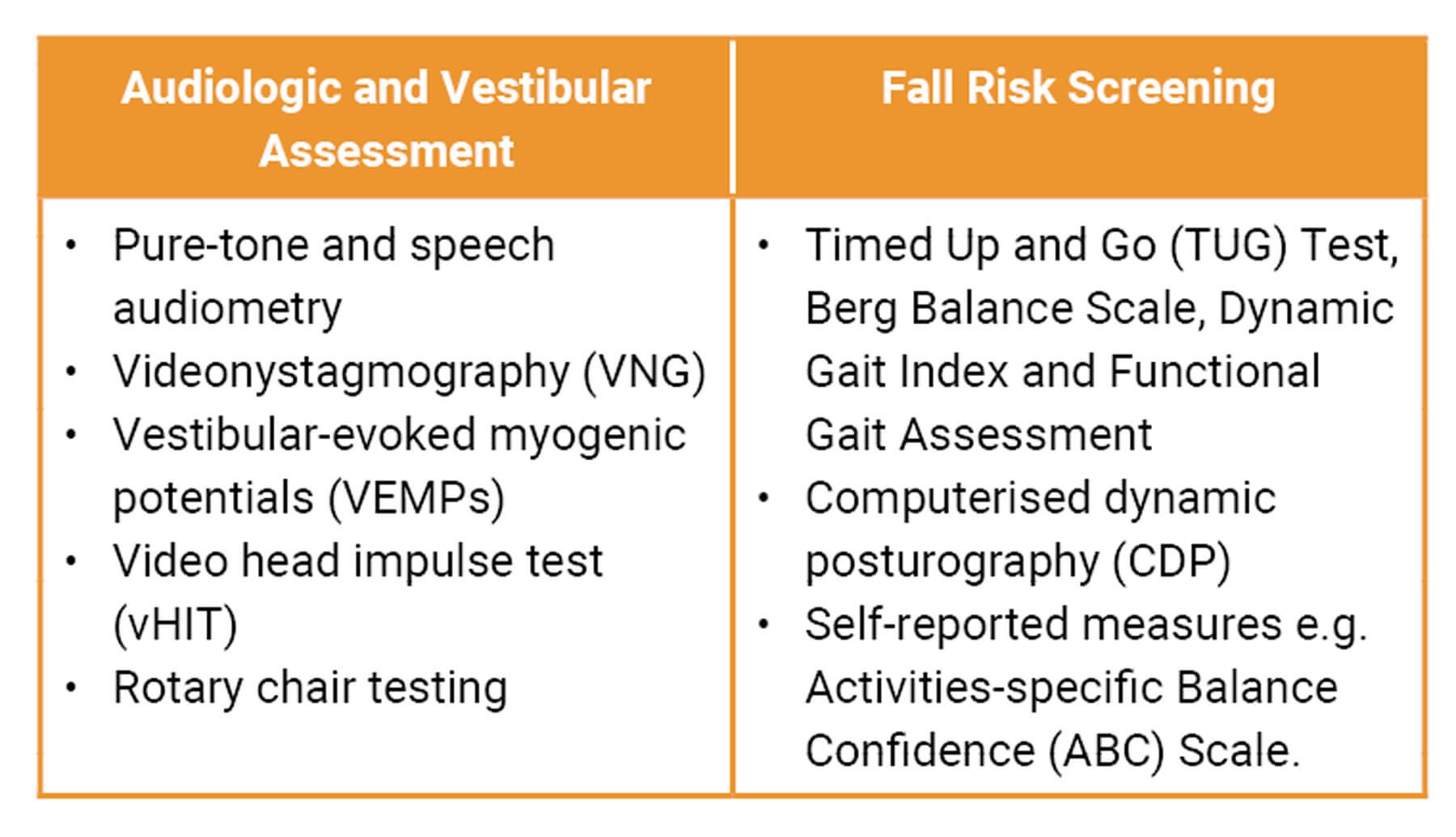
Integrating audiologic, vestibular and functional balance tests allows clinicians to identify high-risk patients and implement personalised interventions. Integrating audiologic, vestibular and functional balance tests allows clinicians to identify high-risk patients and implement personalised interventions.
"Modern hearing aids increasingly integrate accelerometers and gyroscopes, providing automatic fall detection and emergency alerts"
Emerging technologies
Wearable sensors
Inertial measurement units (IMUs) embedded in shoes, belts or hearing aids monitor gait and stability in real time, enablin11g longitudinal risk tracking [17].
Smart hearing aids with fall detection
Modern hearing aids increasingly integrate accelerometers and gyroscopes, providing automatic fall detection and emergency alerts.
Virtual and augmented reality
VR-based rehabilitation provides immersive, task-specific training environments, improving adherence and neuroplasticity [18]. AR solutions may soon allow remote, home-based balance training with clinician oversight.
Artificial intelligence
AI-driven analysis of sensor data can predict fall risk and tailor interventions. Future hearing devices may integrate balance monitoring with advanced speech processing.
Public health and clinical practice implications
Falls cost healthcare systems billions annually, with estimates exceeding $50 billion annually in the US alone [19]. Recognising hearing loss as a modifiable fall-risk factor supports the following recommendations:
- Routine fall-risk screening in audiology and ENT practice.
- Insurance reimbursement for hearing aids, cochlear implants and vestibular rehabilitation as fall-prevention strategies.
- Public awareness campaigns linking hearing health and fall prevention.
- Integrated care pathways fostering collaboration across specialties.
Clinical practice recommendations:
- Screen all older adults with hearing loss for fall risk.
- Encourage consistent use of amplification in individuals with documented hearing loss.
- Refer for vestibular evaluation when balance complaints accompany auditory dysfunction.
- Incorporate dual-task balance training when appropriate.
- Advocate for policy changes that recognise hearing care as part of fall-prevention initiatives.
Future directions
Several avenues warrant further exploration:
- Neurophysiological mechanisms: Advanced neuroimaging (fMRI, EEG) and electrophysiology can clarify how auditory deficits alter multisensory integration.
- Longitudinal studies: Large-scale prospective studies are needed to test whether early amplification or vestibular interventions reduce falls over decades.
- Technology validation: Research should confirm the clinical utility of smart hearing aids, wearable sensors and VR/AR rehabilitation.
- Policy development: Cost-effectiveness studies will strengthen advocacy for broader insurance coverage of hearing and balance interventions.
Conclusion
The relationship between hearing impairment and balance dysfunction is a critical consideration for modern audiologic and otologic practice. Hearing loss increases fall risk through multiple pathways, including shared inner ear pathology, reduced sensory redundancy, increased cognitive load and altered neuroplasticity. Clinicians can mitigate this risk by integrating fall-risk screening, auditory rehabilitation, vestibular therapy and interdisciplinary collaboration into care. Advances in technology and policy provide further opportunities to enhance safety and quality of life. With continued innovation, the integration of hearing and balance health has the potential to transform fall-prevention strategies worldwide.
References
1. World Health Organization (WHO). World report on hearing. Geneva 2021.
www.who.int/publications/i/item/
world-report-on-hearing
[Link last accessed September 2025]
2. Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med 2011;171(20):1851–2.
3. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: A review of the literature. Maturitas 2013;75(1):51–61.
4. Agrawal Y, Carey JP, Della Santina CC, et al. Disorders of balance and vestibular function in U.S. adults: Data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med 2009;169(10):938–44.
5. Rauch SD, Velazquez-Villaseñor L, Dimitri PS, Merchant SN. Decreasing hair cell counts in aging humans. Ann N Y Acad Sci 2001;942:220–7.
6. Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: A review of an emerging area of research. Gait & Posture 2002;16(1):1–14.
7. Lin FR, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med 2012;172(4):369–71.
8. Wayne RV, Johnsrude IS. A review of causal mechanisms underlying the link between age-related hearing loss and cognitive decline. Ageing Res Rev 2015;23(PT B):154–66.
9. Campbell J, Sharma A. Cross-modal re-organization in adults with early-stage hearing loss. PLoS ONE 2014;9(2):e90594.
10. Al-Yahya E, Dawes H, Smith L, et al. Cognitive motor interference while walking: A systematic review and meta-analysis. Neurosci Biobehav Rev 2011;35(3):715–28.
11. Carpenter MG, Campos JL. The Effects of Hearing Loss on Balance: A Critical Review. Ear Hear 2020;41(Supp 1):107S–19S.
12. Rumalla K, Karim AM, Hullar TE. The effect of hearing aids on postural stability. Laryngoscope 2015;125(3):720–3.
13. Viljanen A, Kaprio J, Pyykkö I, et al. Hearing acuity as a predictor of walking difficulties in older women. J Am Geriatr Soc 2009;57(12):2282–6.
14. Agmon M, Lavie L, Doumas M. The association between hearing loss, postural control, and mobility in older adults: A systematic review. J Am Acad Audiol 2017;28(6):575–88.
15. Riska KM, Peskoe SB, Kuchibhatla M, et al. Impact of Hearing Aid Use on Falls and Falls-Related Injury: Results from the Health and Retirement Study. Ear Hear 2022;43(2):487–94.
16. Whitney SL, Alghwiri AA, Alghadir AH. Physical therapy for persons with vestibular disorders. Curr Opin Neurol 2019;32(1):137–44.
17. Salarian A, Horak FB, Zampieri C, et al. iTUG, a sensitive and reliable measure of mobility. IEEE Trans Neural Syst Rehabil Eng 2013;21(2):291–9.
18. Kang GE, Stout A, Waldon K, et al. Digital Biomarkers of Gait and Balance in Diabetic Foot, Measurable by Wearable Inertial Measurement Units: A Mini Review. Sensors (Basel, Switzerland) 2022;22(23):9278.
19. Florence CS, Bergen G, Atherly A, et al. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc 2018;66(4):693–8.
Declaration of competing interests: None declared.











