Benchmarking is a process of comparison between the performance characteristics of separate, often competing, organisations intended to enable each participant to improve its own performance [1]. Often, in healthcare, benchmarking is carried out by central government departments or regional agencies in order to identify gaps in performance and then to centrally manage the organisations in question to close the performance gap.
One may call this process Benchmarking for Accountability. Such a process has its place, but is often not particularly useful in terms of fostering long lasting, positive change in a healthcare setting.
The alternative approach is to undertake Benchmarking for Innovation which provides a safe environment for participating organisations to compare their own performance and share innovations between themselves. In 2011 I discovered a group 10,500 miles away from London who had managed to make this work successfully. It is called The Health Roundtable [2]. The Health Roundtable is a non-profit membership organisation and, at the time of writing, has 148 member hospitals across Australia and New Zealand. It receives no direct government funding. Instead it relies primarily on subscription payments from its members and secondarily on corporate sponsorship.
The Health Roundtable collects a large set of data from each member organisation and produces a series of automated but bespoke benchmarking reports, quarterly, in key areas such as inpatient briefings, departmental reports, emergency comparisons and mortality funnel plots. Through these reports, the Health Roundtable acts as a rapid screening tool for member organisations and helps them to search for the reasons for differences. These differences could be down to data methods, clinical practices or other effects. There are no right or wrong answers and members are not required to take any action as a result of their reports. Of course, many members do take action in order to improve their performance as a result of the information and support they have access to.
One of the key reasons for the success of The Health Roundtable is the Honour Code, which all members are required to sign up to when they join. It clearly states that ‘No member shall criticise the performance of other member hospitals, or use any of the information to the detriment of a fellow member. No external distribution of data or conclusions based on Health Roundtable data is made without the unanimous consent of all participants.’
The Health Roundtable is not just about the data and the benchmarking. The organisation holds over 20 ‘Roundtable’ meetings each year, with between 30 and 120 participants at each one, across topics such as Imaging, Allied Health (including Audiology), Surgical Journey, Patient Safety, Nursing and Mental Health. The Health Roundtable process for spreading innovative ideas draws on the ‘Diffusion of Innovation’ concept of Everett Rogers [3]. At each meeting, participants hear from experts in the topic area, receive a review of their data and share their particular innovations with each other. As The Health Roundtable started in 1995, there is now a repository of nearly 20 years of good practice and innovation presentations available to all members. Additionally one of the other key values of Health Roundtable meetings is the networking opportunity provided at the meetings and in the coffee / lunch breaks. A short video explaining how the meetings work, and giving participants views on a recent meeting is available on The Health Roundtable website [4].
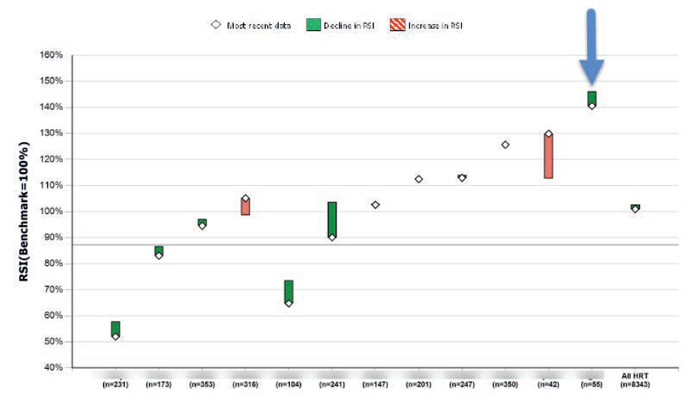
Figure 1: A comparison of risk adjusted length of stay (relative stay index) for under 17 tonsillectomy for 12 hospitals across Australia and New Zealand in Jul-Dec 2013.
As an example relevant to ENT, consider the comparison of data for hospitals in Australia and New Zealand in an example specific to ENT (tonsillectomy patients – under 17 only). The chart in Figure 1 shows a comparison of relative stay index (RSI) (a risk adjusted measure of Average Length of Stay) between 12 organisations. RSI is a good comparative measure, and excessively high values can push up the costs of treatment in public hospitals at a time when healthcare finance is under the spotlight. A hospital executive from the organisation highlighted by the blue arrow would be interested to look at the data further, particularly for the organisations towards the left hand side of the chart (i.e. the ones with lower RSI values) to investigate whether there are specific practices they could adopt to reduce their length of stay and deliver a more efficient and cost effective service.
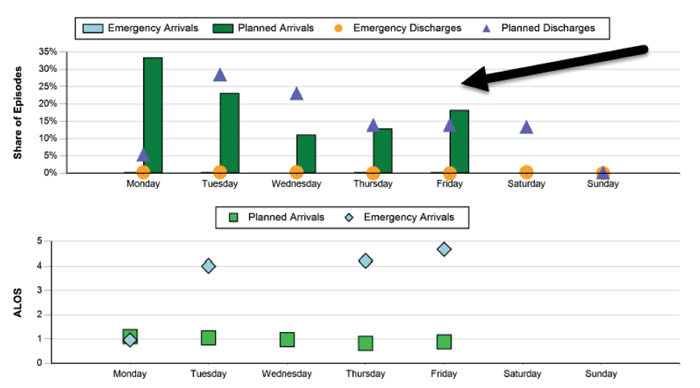
Figure 2: Chart showing arrivals by day of the week for tonsillectomy procedures and a comparison of average length of stay by day of arrival.
Upon closer examination of the data (Figure 2) it can be seen that, for this organisation, there is a disparity between the numbers of planned arrivals by day of the week. This in turn causes a significant difference between the length of stay of a patient between the busy days of the week and the less busy days. Comparison of this data with similar organisations, followed by a phone call to establish alternative practices that could be employed may help this organisation to deliver a more efficient service.
Since first discovering The Health Roundtable in 2011, and having now spent a year living in Sydney, working to develop the organisations’ capabilities and reach further, I remain convinced that Benchmarking for Innovation is an important addition to the strategy of any healthcare organisation to cope with the current and future challenges of a financially constrained environment, workforce shortages, developing technology and an ageing population. Furthermore, there doesn’t currently seem to be an organisation that offers this to hospitals in the National Health Service (NHS) and this seems to be an important gap at present.
References
1. Kay J. Healthcare Benchmarking. The Hong Kong Medical Diary 2007;12:22-7.
2. The Health Round Table.
www.healthroundtable.org
Last accessed July 2014.
3. Rogers E. The Diffusion of Innovations. 4th Edition. The Free Press, 1995.
4. The Health Round Table ‘Sharing Innovations’.
https://www.healthroundtable.org/JoinUs/
AboutUs/VideoSharingInnovations.aspx
Last accessed July 2014.
Declaration of Competing Interests: PW is currently the Director of Operations for The Health Roundtable based in Sydney, Australia which is a non-profit membership group for public hospitals in Australia and New Zealand.




