Musculoskeletal disorders are one of the leading cause of sickness absence from work, work disability and loss of productivity across all European Union member states. Isla Beausire is a working audiologist with a personal and professional interest in this subject area and has worked closely with local health and safety advisors to highlight potential problem areas and to develop possible solutions. In this article she shares her progress so far.
Musculoskeletal disorders (MSDs) are any injury, disorder or damage to tendons, ligaments, muscles, nerves, blood vessels or bones which make up the human musculoskeletal system, resulting in decreased movement and/or pain for the individual.
According to the Health and Safety Executive (HSE), “Work related musculoskeletal disorders (MSDs) are the most commonly reported cause of occupational ill health in Great Britain and account for 41% of all ill health cases and 34% of all working days lost due to ill health” [1].
With these figures in mind and with a personal interest in MSDs, I set out to research these issues within our profession. What I found was one paper by Chantal Brudel for the American Speech-Language-Hearing Association [2], which gave an insight into a day in the life of an audiologist, the tasks she performed and the potential damage she was causing to herself due to the different movements she was making during the course of her working day. What I wanted and needed was information regarding legislation, support and information I could use to help my colleagues and myself with the daily difficulties we were experiencing in our roles as audiologists. Interestingly, this paper also reported that there was little in the way of “ergonomic information specific to the design of audiology work environments”.
There are eight pieces of UK legislation involved with the prevention, management and review of MSDs within the workplace. Each one outlines how employers are responsible for the provision of a safe work environment to minimise the risks posed to the employee during the course of their working day. They also advise that employees have some responsibility for their own safety at work.
Audiology in Shropshire
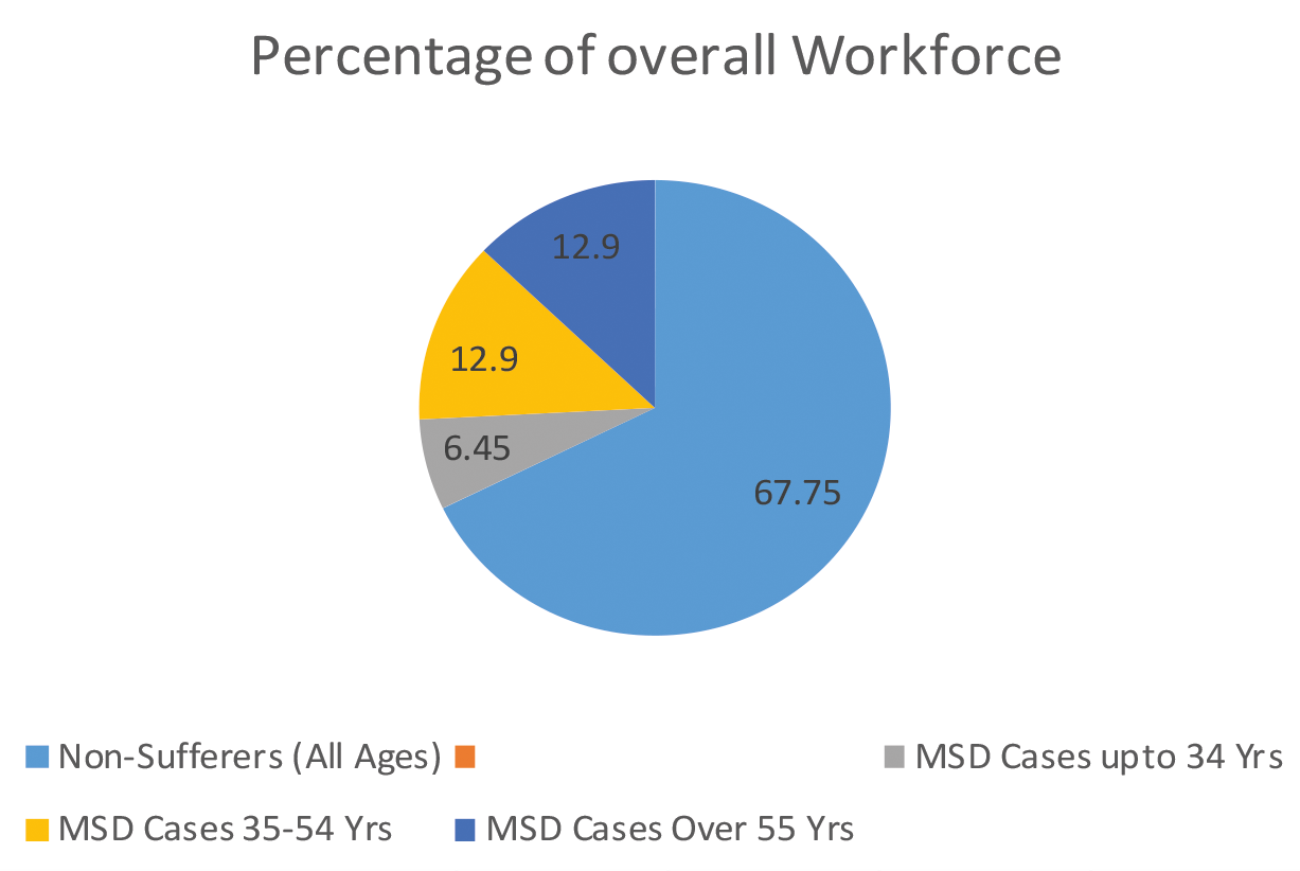
In Shropshire we have 10 members of staff with known MSDs, who are currently being managed under the above legislation. This effectively accounts for 32.25% of our audiology workforce. If we were to assume that this is an average throughout the national audiology community, then 32.25% is a large part of our workforce with long-term physical difficulties needing management and support, possibly caused or exacerbated by, ‘the profession’. The National Office for Statistics reports that we have an ageing population [3], this represents not just our service users, but our workforce too and the Government have also decided that our working lives must extend into our late sixties before we can apply for our state pensions. Interestingly, MSDs are not just the curse of the older audiologist; 12.9% of the Shrewsbury and Telford Hospitals (SATH) audiology staff with MSDs, are nearing retirement age, 6.45% are in their twenties and the remaining 12.9% are in the age range 35-55 (Figures 1-2).
Figure 1. Breakdown of long-term MSD cases within SATH audiology department.
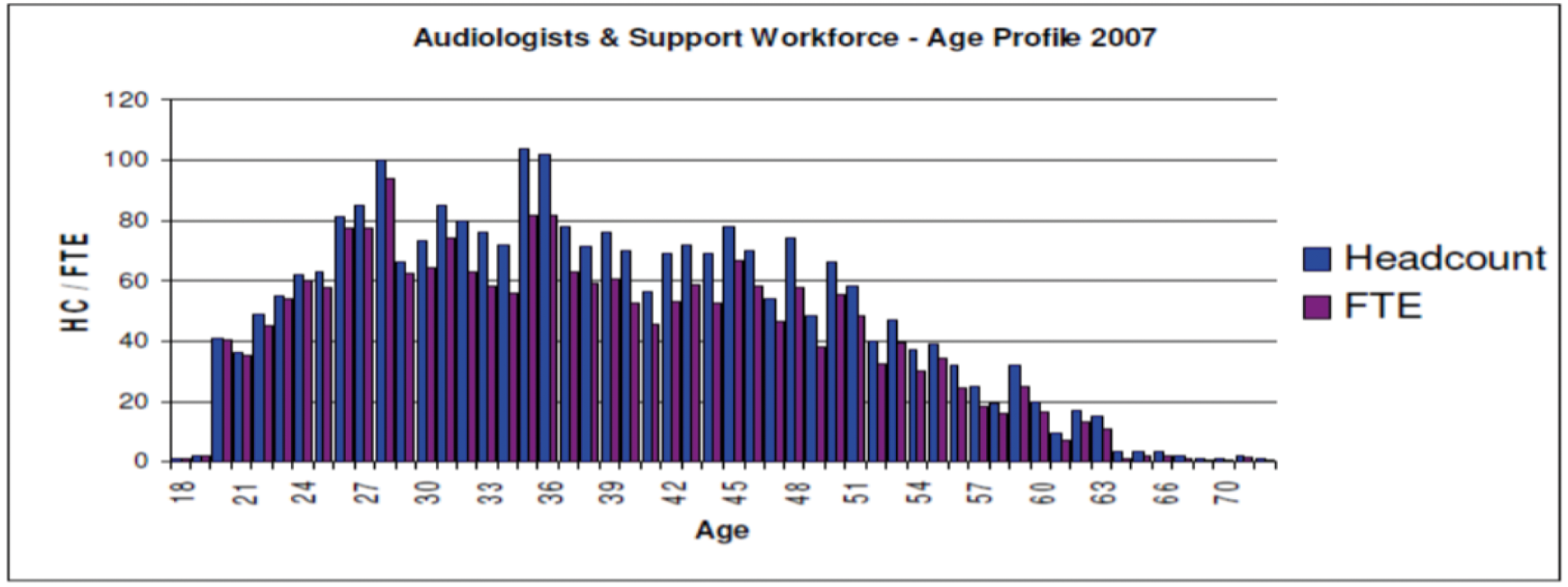
Figure 2. Graphical information shows the range of ages throughout the audiology workforce
in England in 2007 and is taken from the NHS Workforce Review Team [5].
How we tackle MSDs
With the introduction of ‘any qualified provider’ (AQP) and our journey through IQIPS accreditation (‘Improving Quality In Physiological Diagnostic Services’), health and safety has been at the forefront of our daily routine. We have joined forces with our trust health and safety team, in particular the manual handling group, who are helping us ‘fine tune’ our departmental specific training. They have also completed risk assessments for those members of our team who have experienced specific MSD through injury, to determine the best possible management course. Part of the overall management of MSDs was working with each individual member of staff to determine which options were suitable for their needs. In Shropshire we have 13 sites where we provide audiological services, two main sites at Telford and Shrewsbury and the other 11 spread throughout the county. Some members of staff were travelling long distances to their respective clinics, carrying and setting up equipment and also carrying the necessary hearing aid stock to complete their clinic lists. Individual detailed display screen equipment (DSE) and manual handling assessments were carried out at each of the clinics where they worked, to determine the equipment needed.
“With the introduction of ‘any qualified provider’ (AQP) and our journey through IQIPS accreditation (‘Improving Quality In Physiological Diagnostic Services’), health and safety has been at the forefront of our daily routine.”
According to ergo-plus.com, the three primary ergonomic risk factors for MSDs are 1) high task repetition, 2) forceful exertion and 3) repetitive sustained awkward position [4]. All these risk factors are an everyday occurrence for audiology staff. For those members of staff regularly travelling to community clinics, driving position was also considered an ergonomic risk factor.

Figure 3. Identifying the correct desk set up.
For adult audiology clinics we looked at all the possible risk factors, for each member of staff, ascertaining:
- The chair provided adequate support for their neck shoulders and back. It was the correct height and was easily adjustable. It also needed to be on wheels and rotate so that a suitable and comfortable position could be obtained for otoscopy, impression taking, completing real-ear measurements (REMs) etc. In the event where the chair was too large to manoeuvre around the patient, examination stools were also provided.
- The set up on the desk was correct for the user. Keyboard, mouse and screen were all at suitable positions for the user. If not, they were easily adjustable to suit individual needs. It was also noted that from a communication point of view, the repetitive movement of the neck, i.e. from typing to looking at the patient, was another main risk factor, so the set up on the desk was such that it minimised the turning movement (Figure 3).
- For one member of staff a hydraulic desk was purchased to minimise the strain to their spine and to allow varied positions throughout their working day. Ergonomic keyboards, a vertical mouse and voice activated dictation software have also been provided to reduce ‘high task repetition’ whilst typing.
- Storage for stock: adequate storage was provided at community clinics so that large amounts of stock were not being carried by the staff. We were able to utilise the transport service provided in the county, which was mainly used to transport medical supplies and samples between community site, GPs and the main hospitals.
- Equipment provision: audiometers, laptops and REM hardware was purchased for each community site, this was an initial expensive outlay, carried out over a few years, but in the long term has been an excellent solution. The wear and tear on the equipment is minimal, so the equipment is lasting longer and load moving for staff has been greatly reduced. This has also allowed members of staff who lived closer to community clinics, but were unable to carry the equipment, to perform clinics in the community and with a wider range of service users. We have also purchased tympanometers to provide cover for ENT clinics held in the community.
- Smaller, hand held tympanometers have been provided to reduce load moving. Those less portable tympanometers still in use have been put onto trolleys in the clinic rooms, allowing them to be moved more easily – especially useful for paediatric clinics.
- We have also recently been looking into providing more video otoscopes to prevent the bending, stooping and awkward neck rotation whilst performing otoscopy.
- The use of insert phones instead of head phones has been a very useful solution for one member of staff who had difficulty manipulating the tensioners on the headphones. We are looking to provide a set of insert phones for all audiometers at community sites as well; not just for the audiometric value, but for the high task repetition of headphone placement.
- For the moving of small equipment items, we have provided trolleys to reduce carrying items over long distances.
“It is important as professionals, that we work towards providing and maintaining a safe work environment.”
Paediatric clinics posed some different challenges:
- Otoscopy: in paediatric clinics staff were often needed to kneel on the floor to look in children’s ears – we have used gardening kneeling pads to help with this which staff are finding effective. Some members of staff prefer the child to come to them whilst they are sitting, which again works well, but can be dependent upon the child!
- ‘Playing’ with the child during testing – sitting at low level tables during visual reinforcement audiometry (VRA), performance and play audiometry. We have had clinics running with two members of staff to allow change in height working, i.e. ‘taking turns’ or for those members of staff with MSDs, they can remain at the desk and audiometer whilst the other member of staff performs the test/play. The team have found this useful from a peer review point of view, also. We have also utilised students to perform clinical tasks, allowing the clinical supervisor rest periods from their clinical workload.
- The use of insert phones: from a paediatric test point of view, this produces invaluable ear specific information for young children and babies, along with reducing ‘high task repetition’ of headphone use.
The list of supporting and preventative measures is not exhaustive and as a department we continue to work with our staff to find solutions to MSD risk factors and triggers.
In conclusion
It is important as professionals that we work towards providing and maintaining a safe work environment, utilising legislation and local guidelines to support those members of staff who have developed MSDs and for those who could develop MSDs in the future. Regular assessments and reviews of practice, not only clinically, but for posture and DSE use are also vitally important to maintain our workforce.
References
1. Guidance – Musculoskeletal Disorders. Available at:
www.hse.gov.uk.
2. Trudel C. Ergonomic Case Study of an Audiologist performing Visual Reinforcement Audiometry. American-Speech-Language-Hearing-Association; 2014.
3. The Office of National Statistics. Revised population estimates for England and Wales: mid-2012 to mid-2016. Available at:
www.ons.gov.uk/peoplepopulationandcommunity/
populationandmigration/populationestimates/
bulletins/annualmidyearpopulationestimates/
mid2012tomid2016
4. The definition and causes of Musculoskeletal Disorders (MSDs). Available at:
https://ergo-plus.com
5. NHS Workforce Review Team. Workforce summary: Audiologists (England only). 2008.