Introduction
In January 2014, Professor Mark Drakeford, Minister for Health and Social Services, defined Prudent Healthcare as, “Healthcare that fits the needs and circumstances of patients and actively avoids wasteful care that is not to the patient’s benefit.” ‘Prudent’ healthcare delivers three objectives:
- Doing no avoidable harm
- Carrying out the minimum appropriate intervention that delivers the outcome valued by the patient
- Promoting equity between those people who use it and those providing services.
In health services across the world around 10% of patients admitted to hospital experience some degree of avoidable harm. Across the world, 20% of all work done by the health service does not positively affect outcomes. There is evidence that only 18% of patients’ time spent in healthcare environments provides any value to them with the rest spent waiting for the next step in the process. Currently, very few services are commissioned on the basis of delivering outcomes valued by patients. Instead, many health services are arranged around the needs of the system or of those delivering rather than those paying for and receiving healthcare.
Imprudent healthcare can result from:
- Habitual practice of clinicians and patient expectation of ‘being fixed’
- The causes of harm being known but complex to eradicate
- Professional autonomy leading to inappropriate variation in outcomes and experience
- High reliability, high quality care, taking time and resource to embed in practice
- Response to increasing demand has been to do more of the same or put patients on waiting lists
- Healthcare policy and measurement focuses on procedures rather than outcomes or experience
- Patients are not routinely informed about or engaged in making decisions
- Care is not person-centred
- Policies and rules get in the way of delivering good outcomes and experience
- Management information does not show what is happening ‘on the ground’.
Background
To make services ‘Prudent’, health services must focus on delivering outcomes and experience valued by patients and improving ‘flow’ through the system. Data that measures outcomes, experience and flow needs to be collected to allow appropriate decisions to be made with citizens about commissioning and performance. This ensures that organisations are focused on delivering what really matters to the people they serve.
To change service delivery, clinicians training and time must be allocated to deliver better outcomes and experience within a culture of continuous improvement. This means that clinicians must believe that they are responsible for ensuring people are fully informed and engaged in making decisions about their health and well being, that patients receive high quality support and care, based on the best available knowledge.
An important principle is that the people using services need to understand their personal responsibilities as citizens. This includes being involved in decisions about commissioning and design of services. Patients also need training to work with clinicians to set personal goals and expectations of treatment. The use of simple ‘option grids’ can set out benefits and risks of choosing between different treatments. In emergency circumstances it may not always be possible for people to be fully involved in, or aware of, decisions that have to be made in their care. But for the overwhelming majority of healthcare interactions, there is a shared responsibility between the people receiving and the people delivering healthcare.
Prudent audiology workshop
A workshop was held in Swansea to test these prudent principles in audiology and see how they could be applied. This workshop considered the adult hearing loss, tinnitus and dizziness / imbalance services provided by Abertawe Bro Morgannwg University (ABMU) Health Board.
Audit demonstrated that around 25% of ENT outpatient referrals are currently for patients with hearing loss, dizziness and tinnitus. Very few of these receive medical or surgical treatment but are seen in ENT outpatient clinics and then referred to audiology for management. Issues in audiology services across Wales include long waiting times for re-accessing services and the fitting of hearing aids to one ear only.
The prudent healthcare workshop held in ABMU highlighted the following barriers that were felt to apply in audiology services:
- A survey from the National Institute for Health and Care Excellence identifying barriers to the implementation of guidelines notes the commonest problem was difficulty in getting consensus amongst colleagues.
- There is an expectation that clinicians do ‘something’ just because they feel they must be seen to be doing something.
- Capacity may in some instances drive demand. Short waiting lists get referred to following the principle of ‘build it and they will come’. Hyper-specialisation of service delivery can in some cases lead to a lack of clarity as to who is taking an overview of the patient, particularly where a patient has multiple concurrent health problems.
In the workshop, the application of prudent healthcare principles to an audiology service were described:
Co-create health with the public, patients and partners
Waste and duplicate referrals in the current system suggest co-creation of a new pathway:
- Agree criteria with general practitioners (GPs) for e-referral of adult and child patients with hearing loss, balance disorder and tinnitus direct to audiology
- Exclude conditions requiring medical or surgical treatment
- All referrals to be considered by an appropriately qualified audiologist with the expectation that less than 2% will be directed to ENT
- Agree referral by audiology for imaging
- Agree support from neuro-radiology
- Agree onward referral pathways.
Do no harm
- Routine audit and discussion with ENT
- All patients needing medical or surgical input must be seen in ENT
- Report any adverse incidents from missed pathology
- Patients must always be seen in ENT if that is their preference
Attention must be paid to minimising patient distress.
Do the minimum appropriate to achieve the desired outcomes
- Potential to release resources in ENT outpatient clinics, surgical intervention, diagnostic tests
- Improve delivery of outcomes valued by the patient, better hearing, less dizzy, reduced tinnitus distress
- Change skill mix in audiology, using more assistants and more advanced practitioners
- Ensure patients maintain independent living.
Choose the most prudent care, openly together with the patient
- Use the Co-creating Health Framework
- Use option grids in communications with patients
- High quality service meeting or exceeding standards
- Small number of patients may choose to have medical or surgical intervention
- Significant number of patients may choose not to have any intervention
- Patients must be reviewed and reassessed at their request
- Prudent service should be financially attractive for both the National Health Service (NHS) organisation and the Commissioner.
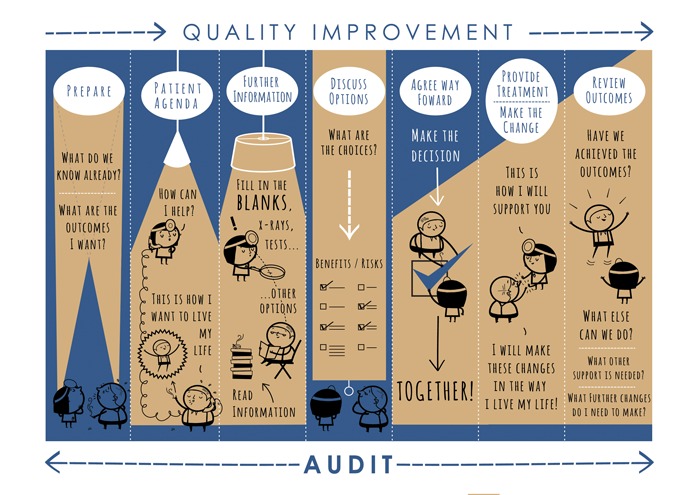
Figure 1: Co-creating health framework.
Conclusion
The ABMU workshop identified five main ideas to improve audiology services using the prudent healthcare principles. These were:
- Walk-in open access clinics for the public who have hearing loss or tinnitus (two groups). Clinics would be provided in accessible locations close to people’s homes and be led and delivered by audiology and would be a one stop shop for:
• information: resources, support, clinical conditions, prevention, self-help
• advice: tinnitus management, care of hearing aids, ear hygiene, etc
• equipment: hearing aids, batteries, spare parts. - Rapid access models with the more appropriate use of technology, linking primary and secondary care better using telephone virtual clinics, perhaps for a cluster or GP practices at the same time.
- A treatment pathway for patients with ear wax problems to provide a single consistent service, manage referrals across primary and secondary care, reduce inappropriate referrals to ENT, and improve access and outcomes for the patient.
- A one-stop clinic for managing balance disorder and dizziness including routine balance rehabilitation provided by audiologists with referral mechanism for complex cases.
- Applying a co-creating health framework that supports clinicians to engage patients in making decisions about their own options (Figure 1). The framework includes the use of option grids (Figure 2).
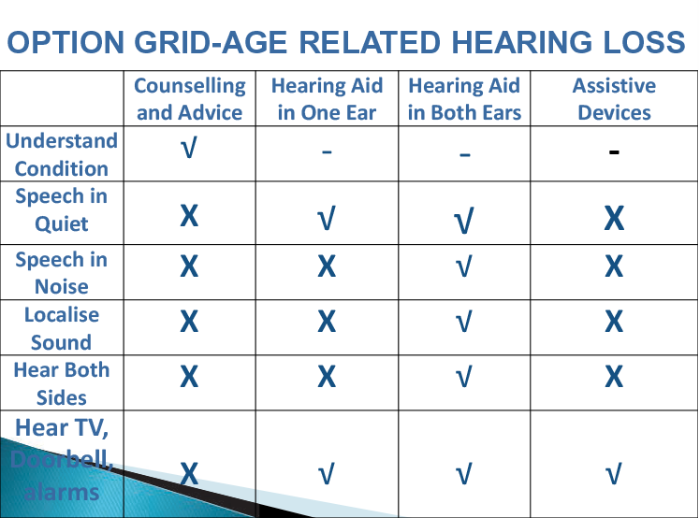
Figure 2: Option grid age-related hearing loss.
Declaration of Competing Interests: None declared.