Many professions, such as law, accounting, engineering and some areas of healthcare charge hourly rates in a fee-for-service model. Administratively, this can be a challenge to track hours, bill clients/patients, and collect payment, but this does lend toward greater transparency and promotes better understanding of the value of the professional services included with any final work-product. In this article, Dr Spoor details this fee-for-service ‘unbundled’ approach.
The term ‘unbundling’ is a buzzword in the profession of audiology in the United States (US). This term refers to separating fees charged for professional services from the fees associated specifically with products (e.g. hearing aids) provided by the audiologist.
For a number of recent years, US-based practice owners have debated moving to this alternative pricing structure, state conferences have well-known clinicians debate the model, and national and international conferences highlight keynote presentations about unbundling fees from the sale of a product in provision of hearing care. While the concept is not new within medicine, nor audiology, unbundling is a paradigm shift for practices that prescribe, dispense, fit, and sell hearing aids.
Prior to the late 1970s, audiologists (in the US) did not sell hearing aids, citing ethical reasons. Rather, the audiologist would complete a comprehensive diagnostic evaluation and recommend (now, the required term is ‘prescribe’) the make, model, and features necessary for the hearing aid to be purchased by the patient. The patient would then purchase the hearing aid from a hearing aid dispenser, and would (sometimes) return to the audiologist to verify the function and benefit of the hearing aid. This unbundled approach – paying for the diagnostic testing, hearing aid evaluation, and follow-up verification – changed when audiologists began selling hearing aids in-office, eliminating the hearing aid dispenser. When audiologists offered a one-stop-shop for diagnostic testing, hearing aids, and the associated fitting, the pricing system changed from the unbundled model to a bundled model, where all professional services are subsumed in the cost of the device itself. Most dispensing audiology practices still use a bundled model today [1].
Are audiologists listening?
The National Academies of Science, Engineering and Medicine (NASEM) 2016 report, ‘Hearing Health Care for Adults’, cited the cost of a pair of hearing aids at $4700 [2]. This cost can scare many potential patients. In addition, poor hearing aid adoption rates continue around the world: in 2014, only 42% of individuals who could benefit from a hearing aid in Norway used one, and as few as 14% of individuals in Japan [3]. The cost of (bundled) hearing aids has been cited multiple times as one of the key barriers to the lack of adoption, most recently in the MarkeTrak survey from 2022 [4]. Consumer groups also report (bundled) hearing aid costs as a barrier to purchase [5,6]. Reducing the upfront cost of a hearing aid purchase by offering an unbundled pricing model can eliminate one of the main concerns from individuals for lack of hearing aid adoption.
Make the change
The process of changing from a bundled to unbundled pricing model is not difficult conceptually, but does take time and preparation. A realistic timeframe to implement this pricing change is 6–12 months and requires commitment from all individuals with patient interaction, from front-office personnel to providers. Audiologists who consult specifically on unbundling recommend a step-by-step process:
- Determine the practice’s hourly rate (break-even plus profit).
- Assign prices to all hearing aids services based on the hourly rate and average appointment time.
- Set appointment prices after reviewing all insurance contracts that offer hearing aid service coverage.
- Determine (create) if an optional Service Plan will be offered. (Service plans offer the patient the ability to pre-purchase coverage for hearing aid services over a set period, typically one to three years.)
- Modify scripts, from the front office’s intake to provider counselling, to confirm the messaging to patients.
- Publish the pricing change via marketing media (e.g. website).
Unbundling benefits
The initial time and effort to switch to an unbundled pricing model may cause pause, but the benefits of unbundling are significant. First, and most importantly, new research is showing the harm of untreated hearing loss, including increased risk of falls [7], social isolation [8], depression [9], and dementia [10]. Hearing healthcare providers must focus on patient outcomes, including diminishing hearing loss comorbidities, and offer options that allow individuals with hearing loss to purchase amplification. Reducing the initial price of hearing aids by offering an unbundled price can allow more individuals to proceed with hearing aids at a lower (upfront) cost compared to bundled models.
Second, unbundling offers the patients transparency around the cost of hearing aids and associated services. A need for greater transparency was also identified in the NASEM 2016 report [2]. Audiology practices should desire to clearly identify to the purchaser the cost of a hearing device separate from the hearing aids services around verification and validation. The cost of hearing aid services will be commensurate with the level of education of the provider. Practices that employ audiologists who have obtained a clinical doctorate (e.g. Doctor of Audiology, AuD) will naturally have a higher hourly rate compared to those who have providers only trained in the testing for and fitting of hearing aids. However, at least one study in 2022 suggests patients are willing to pay more for (perceived) quality care [1,2]. Transparency goes hand-in-hand with value. The value of a $4700 pair of hearing aids is significantly different than a $2000 pair of hearing aids with $2700 of hearing aid services (fitting and long-term follow-up). Additionally, the value of the provider is demonstrated in the unbundled pricing model, as they charge for their time and expertise.
Finally, unbundled pricing mimics the medical system. Outside the US hospital systems, physicians are paid on a fee-for-service basis. Patients are required to pay for services at the time they are rendered. The unbundled hearing aid model mirrors this system. Practices offering medical, audiologic, and hearing aid services will all be consistent in their model. For practices that market their services to other medical providers (e.g. for collaboration), the unbundled model promotes consistency and a mutual understanding.
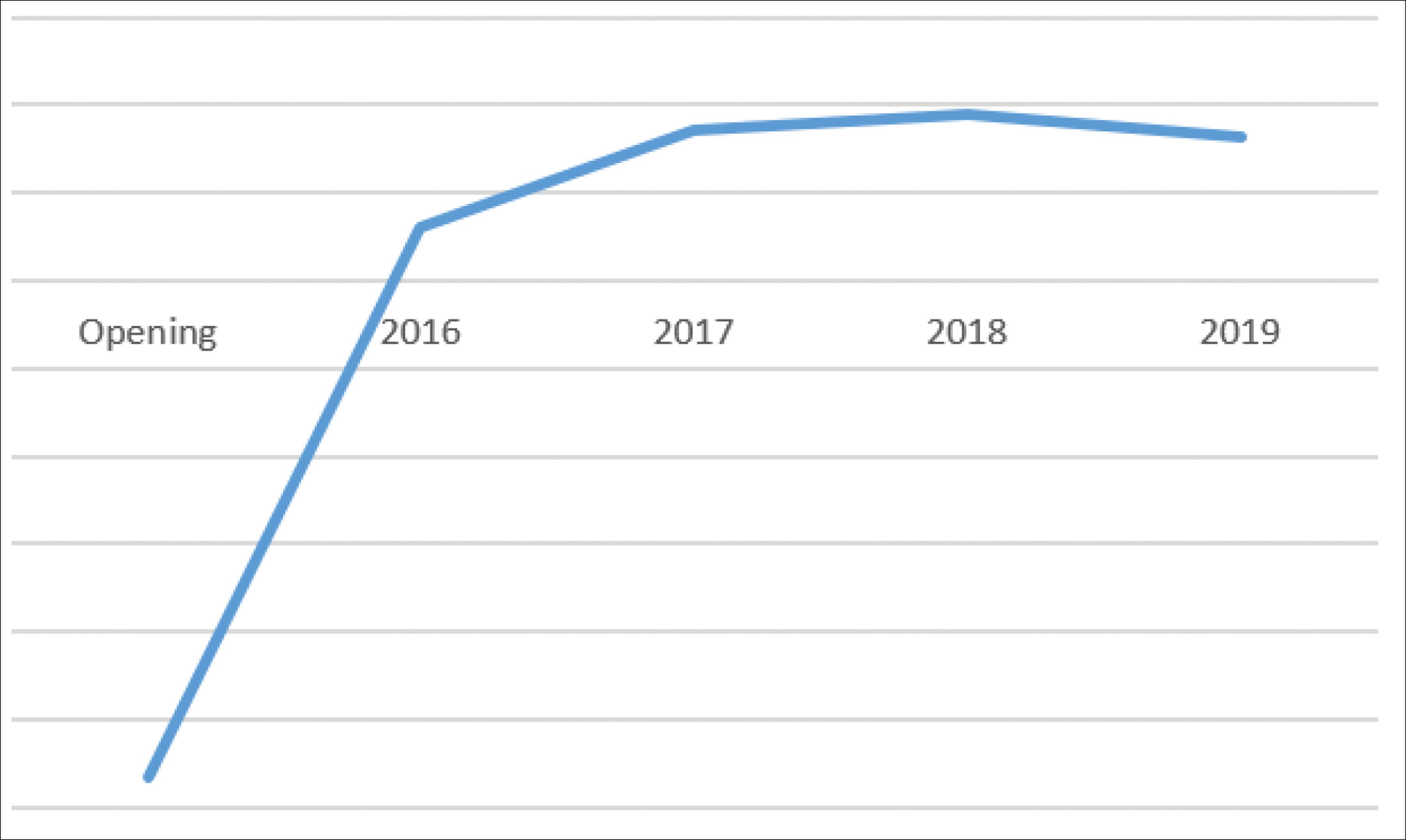
Graph 1: One US private practice that opened with an unbundled model
saw a significant increase in gross income over a five-year period.
Economic advantage
Every healthcare-related business must make money to provide patient care. Unbundled pricing promotes a more consistent cashflow. Bundled hearing aid prices require the patient to prepay for long-term care, which means each time a patient returns to the office, the appointment does not generate income on that date of service. This bundled model lends itself to entire days without any collection of money, due to the patient having prepaid for services. An unbundled pricing model provides a more consistent cash flow and accurate description of services rendered on each day. Separating long-term hearing aid services from the initial purchase also ensures patients are responsible for their role in the rehabilitation process. Providers who work with complex patients will be compensated for the additional time. Graph 1 shows one US private practice who opened initially with an unbundled model and the growth (gross income) over a five-year period.
Conclusion
An unbundled hearing aid pricing model has many advantages, including transparency, value, and more consistent cashflow. The process of transitioning from a bundled to unbundled practice will take time and dedication, but removing a cost barrier to the adoption of hearing aids benefits the patient and the practice. Additionally, the business of hearing care is based on trust, and the transparency inherent in the unbundled model described here promotes that sense of trust with patients.
References
1. Cox R. 20Q: Hearing aid provision and the challenge of change. AudiologyOnline. 2021
www.audiologyonline.com/articles/
20q-hearing-aid-provision-and-12596
2. National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Sciences Policy, et al. Hearing Health Care for Adults: Priorities for Improving Access and Affordability. Washington, DC, USA; The National Academies Press; 2016.
3. Hidekazu A. Thinking about hearing aid adoption in Japan. Audiology Worldnews. 2014.
www.audiology-worldnews.com/market/
1370-thinking-about-hearing-aid-adoption-in-japan
4. Windmill IM. The Financing of Hearing Care: What We Can Learn from MarkeTrak 2022. Semin Hear 2022;43(4):339–47.
5. Evertt C. Only 1 in 6 Americas with Hearing Loss Wears Hearing Aids – Here’s Why. 2023.
www.ncoa.org/adviser/hearing-aids/
low-hearing-loss-treatment-reasons
6. Hochman A. Over-the-Counter Hearing Aids: Good News, With Some Complications. 2023.
www.webmd.com/a-to-z-guides/
features/fda-otc-hearing-aids
7. Johns Hopkins Medicine. Hearing Loss Linked to Three-Fold Risk of Falling. 2012.
www.hopkinsmedicine.org/news/
media/releases/hearing_loss_linked
_to_three_fold_risk_of_falling
8. Shukla A, Harper M, Pedersen E, et al. Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngol Head Neck Surg 2020;162(5):622–33.
9. Li CM, Zhang X, Hoffman HJ, et al. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005-2010. JAMA Otolaryngol Head Neck Surg 2014;140(4):293–302.
10. Johns Hopkins Medicine. The Hidden Risk of Hearing Loss.
www.hopkinsmedicine.org/health
/wellness-and-prevention/
the-hidden-risks-of-hearing-loss
11. Lagasse J. Consumers willing to pay more for quality healthcare, survey finds. 2022.
www.healthcarefinancenews.com/
news/consumers-willing-pay-more
-quality-healthcare-survey-finds
[All links last accessed November 2023]
Declaration of competing interests: Alicia Spoor has been a paid speaker at state, national, and international conventions/conferences on the topic of unbundling. She offers coaching and consulting services in the area of unbundling as part of her private practice offerings.









