The set of symptoms described as Meniere’s disease may have several causative factors. Timothy Hain and Patthida Maroongroge look for a relationship in the literature between Meniere’s disease and hypothyroidism.
Meniere’s disease (MD) affects around two in 1000 people and is one of the most common causes of dizziness deriving from the inner ear. Although MD is nearly always accompanied with endolymphatic hydrops (See Figure 1), temporal bone studies find hydrops in a far greater proportion of normal temporal bones than would be expected from the prevalence of Meniere’s disease in the population.
Accordingly, the aetiology of MD is believed to be multifactorial. Metabolic and endocrine dysfunction, as well as autoimmune disturbance, have been suggested to be contributing factors to causation of MD. In particular, there is evidence in the literature that thyroid disorders, specifically hypothyroidism and autoimmune thyroiditis, play a role in MD [1-3, 5].
Hypothyroidism is a common endocrine problem in which the thyroid gland fails to produce sufficient thyroid hormone, leading to reduced body metabolic functions. Previous researchers evaluating metabolic factors in MD proposed that hypothyroidism is the aetiology of MD in a small proportion of the cases. In 1978, Powers found that 17 of 98 patients with MD were hypothyroid, and in three of these patients, symptoms of MD were successfully controlled by thyroid hormone therapy alone [1]. Powers suggested that thyroid hormone deficiency was responsible for symptoms of MD in these patients. However, other investigators later did not support this idea as they found low prevalence of hypothyroidism in patients with MD. Kinney reported that only two of their 180 patients with MD had hypothyroidism [2]. Therefore, it is unlikely that hypothyroidism, per se, is a cause of MD.
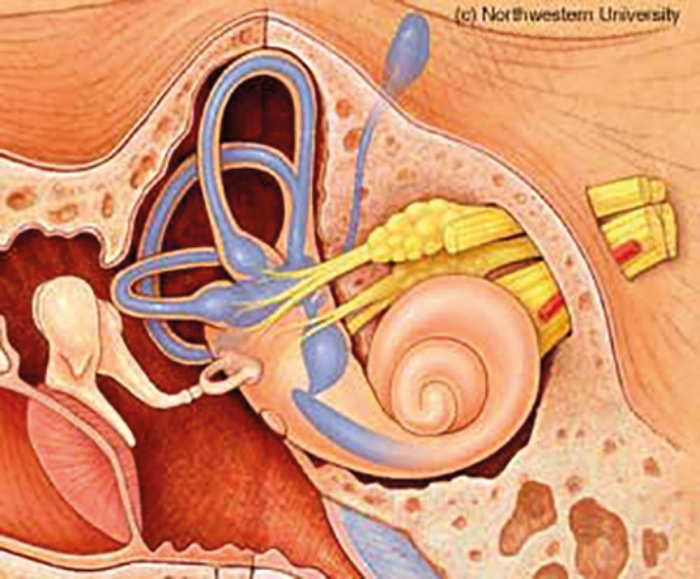
Figure 1a. Normal membranous labyrinth.
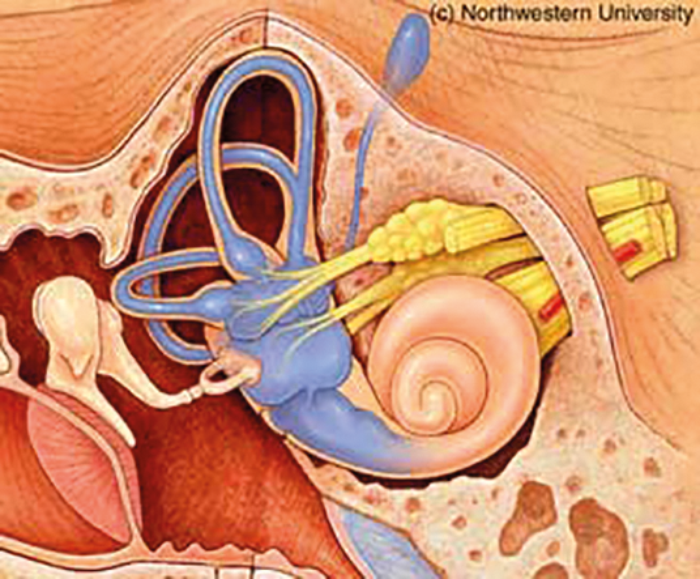
Figure 1b. Dilated membranous labyrinth in Meniere’s disease (Hydrops).
Additional evidence that the thyroid may play a role in MD came from the study of Brenner and associates in 2004 [3]. They reported that the proportion of treated hypothyroidism was 32% in the group of 50 patients with MD, as opposed to 4% in the control group. In addition, the prevalence of thyroid hormone supplement use was even higher (50%) in MD patients older than 60 years old. In the US and other countries where there is no iodine shortage, autoimmune thyroiditis, also known as Hashimoto’s thyroiditis (see Figure 2) is the most common cause for hypothyroidism [4]. Because none of the patients in this study had a history of iatrogenic hypothyroidism, such as thyroidectomy, it was assumed that the cause of their thyroid hypofunction was autoimmune thyroiditis [3].
“The proportion of treated hypothyroidism was 32% in the group of 50 patients with MD, as opposed to 4% in the control group.”
The association between MD and autoimmune thyroiditis was later supported by a study on thyroid autoimmunity and MD [5]. By conducting thorough serum thyroid tests including thyroid auto-antibody tests, Fattori et al found that 38% of 50 patients with MD had autoantibodies to thyroid proteins. This number was significantly higher than those in healthy controls (7%). The most common thyroid autoantibody found in patients with MD was antithyroid peroxidase antibody, followed by antithyroglobulin antibody. Thus, recent studies strongly support an association between MD and autoimmune thyroiditis.
So what is the relationship between autoimmune thyroid disease and MD? It seems unlikely these antibodies both attack the ear and thyroid, as there are several different thyroid auto antibodies associated with MD. One possibility is that there is a shared underlying cause. Autoimmune thyroiditis is a common condition that is often associated with other autoimmune diseases [4]. In the study by Brenner and associates [3], four patients who were taking thyroid supplements had also been diagnosed with systemic autoimmune diseases.
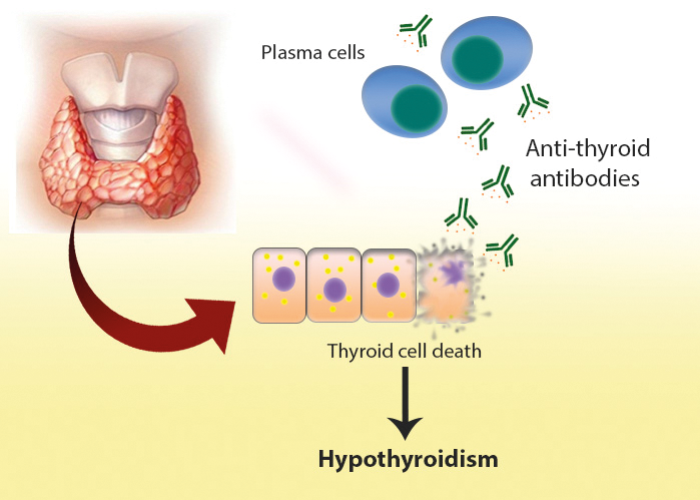
Figure 2. Hashimoto’s thyroiditis.
Brenner and colleagues suggested that autoimmune thyroiditis was unlikely to be a direct cause of MD in these patients, but rather that it was a manifestation of an autoimmune disturbance, that also causes MD. Furthermore, if the auto-antibodies were a direct cause of MD, one would expect that the level of the auto-antibodies would be correlated with the severity of MD. This was not found; in the study by Fattori et al, there was no correlation between pure tone average score and the thyroid auto-antibody titers [5].
Conclusion
Recent studies suggest that there is an association between MD and hypothyroidism, especially hypothyroidism that is a result of autoimmune thyroiditis. This association seems to be related to an autoimmune mechanism rather than reduced thyroid hormone. It is possible that in many cases of MD, autoimmune thyroid disease shares a common underlying autoimmune aetiology with MD.
“The association between MD and hypothyroidism seems to be related to an autoimmune mechanism rather than reduced thyroid hormone.”
Clinical implications
- There is a higher prevalence of autoimmune thyroid diseases in patients with MD compared to the general population.
- Clinicians might consider screening for thyroid autoantibodies in patients with MD as thyroid autoantibodies are very common in this population, and a positive test may suggest that their patient may have an autoimmune cause of their disorder.
- In patients who have MD and who are not on thyroid supplements, thyroid function screening may discover undiagnosed thyroid disorders, especially in older patients as their clinical symptoms are usually subtle thus may be overlooked.
References
1. Powers WH. Metabolic aspects of Meniere’s disease. Laryngoscop 1978;88(1 Pt 1):122-9.
2. Kinney SE. The metabolic evaluation in Meniere’s disease. Otolaryngol Head Neck Surg (1979) 1980;88(5):594-8.
3. Brenner M, Hoistad DL, Hain TC. Prevalence of thyroid dysfunction in patients with Meniere’s disease. Arch Otolaryngol Head Neck Surg 2004;130(2):226-8.
4. Genetics Home Reference. 2017. Hashimoto thyroiditis.
https://ghr.nlm.nih.gov/condition/hashimoto-thyroiditis#diagnosis
Last accessed April 2017.
5. Fattori B, Nacci A, Dardano A, et al. Possible association between thyroid autoimmunity and Meniere’s disease. Clin Exp Immunol 2008;152(1):28-32.
Declaration of competing interests: None declared.