From candidacy to surgery and rehabilitation, cochlear implant practice is evolving, with new technologies shaping outcomes for patients worldwide.

Image courtesy of MED-EL.
Cochlear implants restore a sense of hearing in the profoundly deaf, representing the most successful neuroprostheses available, in terms of both clinical efficacy and value for money. The first multichannel cochlear implants were implanted in 1977, and there are now over one million cochlear implant recipients worldwide.
The principle of restoring a sense of hearing through electrical stimulation has not changed since 1977, but new discoveries and developments have influenced current practice, which continues to evolve in the domains of cochlear implant candidacy (preoperative), surgery (operative) and rehabilitation (postoperative), or optimising patients’ use of the implant.
Candidacy
Cochlear implant candidacy has evolved considerably. It was previously felt that only profoundly deaf patients would benefit. Soft surgical techniques and minimally traumatic electrodes now mean that residual low-frequency hearing, as well as balance function, can be preserved – at least in the short to medium term. This has led to broadened criteria for cochlear implantation in children and adults. In the UK, where candidacy is directed by NICE TA566 [1], the guidelines changed in 2019 to allow more patients to benefit. Significantly, the benchmark for speech recognition scores was changed from Bamford-Kowal-Bench sentences (a measure of functional hearing) to Arthur Boothroyd words (a measure of acoustic hearing), as it was felt that patients with poor hearing but excellent communication strategies might score highly on BKB sentence testing, preventing them from falling into cochlear implant candidacy.
"Cochlear implants restore a sense of hearing in the profoundly deaf, representing the most successful neuroprostheses available, in terms of both clinical efficacy and value for money"
Other ways in which candidacy has evolved include its expansion into single-sided and asymmetric hearing losses, although cochlear implantation for these indications is currently not funded by the National Health Service (NHS). Candidacy has also broadened through the safe and efficacious implantation of older adults, as well as the development of better preoperative assessment tools in audiology and imaging. These advances allow multidisciplinary teams to make robust and responsible decisions about individualised recommendations for cochlear implantation.
Preoperative patient pathway
Preoperative preparation for a cochlear implant can optimise postoperative outcomes. This means that counselling, expectation management and preoperative listening therapy are key. Hearing through a cochlear implant is different from natural hearing and requires careful and responsible consideration before going ahead. Having the opportunity to meet an implant recipient can also be useful, as recommended by the British Cochlear Implant Group Quality Standard 2023 [2]. Preoperatively, patients can also express a preference for a particular device, and they may base their choice on factors such as electrode design, MRI compatibility, aesthetics, streaming and connectivity, and other features including the potential for remote programming. Preoperative decision making is carried out between the patient and a multidisciplinary team including audiologists, surgeons, speech therapists, rehabilitationists, teachers of the deaf and psychology.
Surgical practice
‘Soft surgery’ optimises the potential preservation of residual hearing and the avoidance of vestibular disruption during cochlear implantation. The surgeon avoids disrupting the middle and inner ear structure and integrity during access, deploying a slow and smooth insertion of the electrode to minimise intracochlear turbulence and to avoid disruption of the delicate neural structures. Several recent advancements are based on this concept, including the use of robotic-assisted electrode insertion, image-guided insertion and real-time electrophysiological feedback to monitor cochlear function during electrode insertion.
Another important advancement in surgical technique is the use of local anaesthesia, either with or without sedation, for cochlear implant surgery. This enables patients who are either unfit for general anaesthesia, or who would prefer not to have a general anaesthetic, to receive a cochlear implant. Local anaesthetic surgery is safe, tolerable for most adult patients, and is a key factor in accessibility to cochlear implantation. Awake cochlear implant surgery presents challenges for both patient and surgeon; it therefore requires experience in the technique, and careful preoperative counselling. Although the procedure is not painful, patients can feel the vibration of the surgeon’s drill during surgical access.
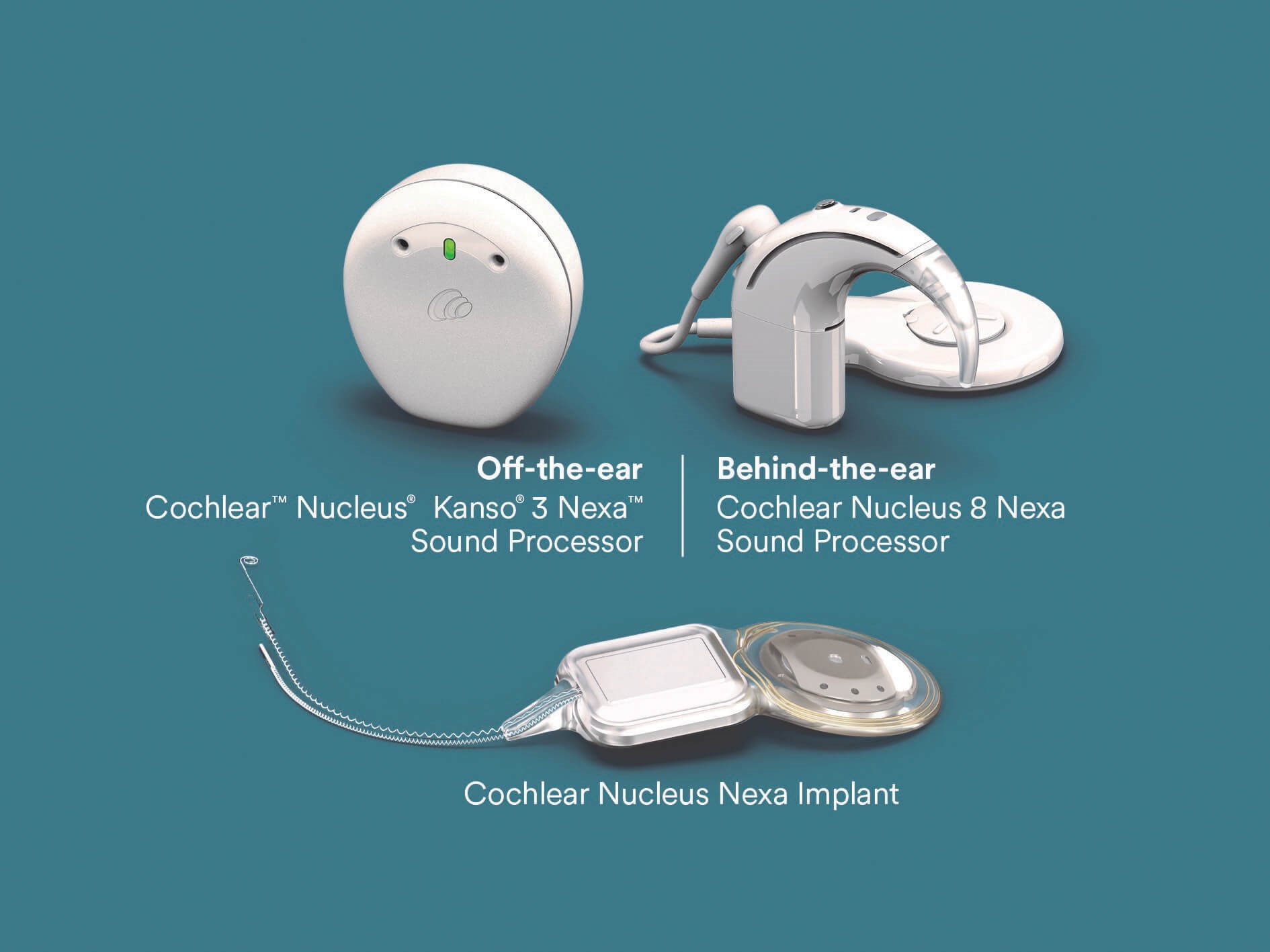
© Cochlear Limited 2025. Image courtesy of Cochlear Limited.
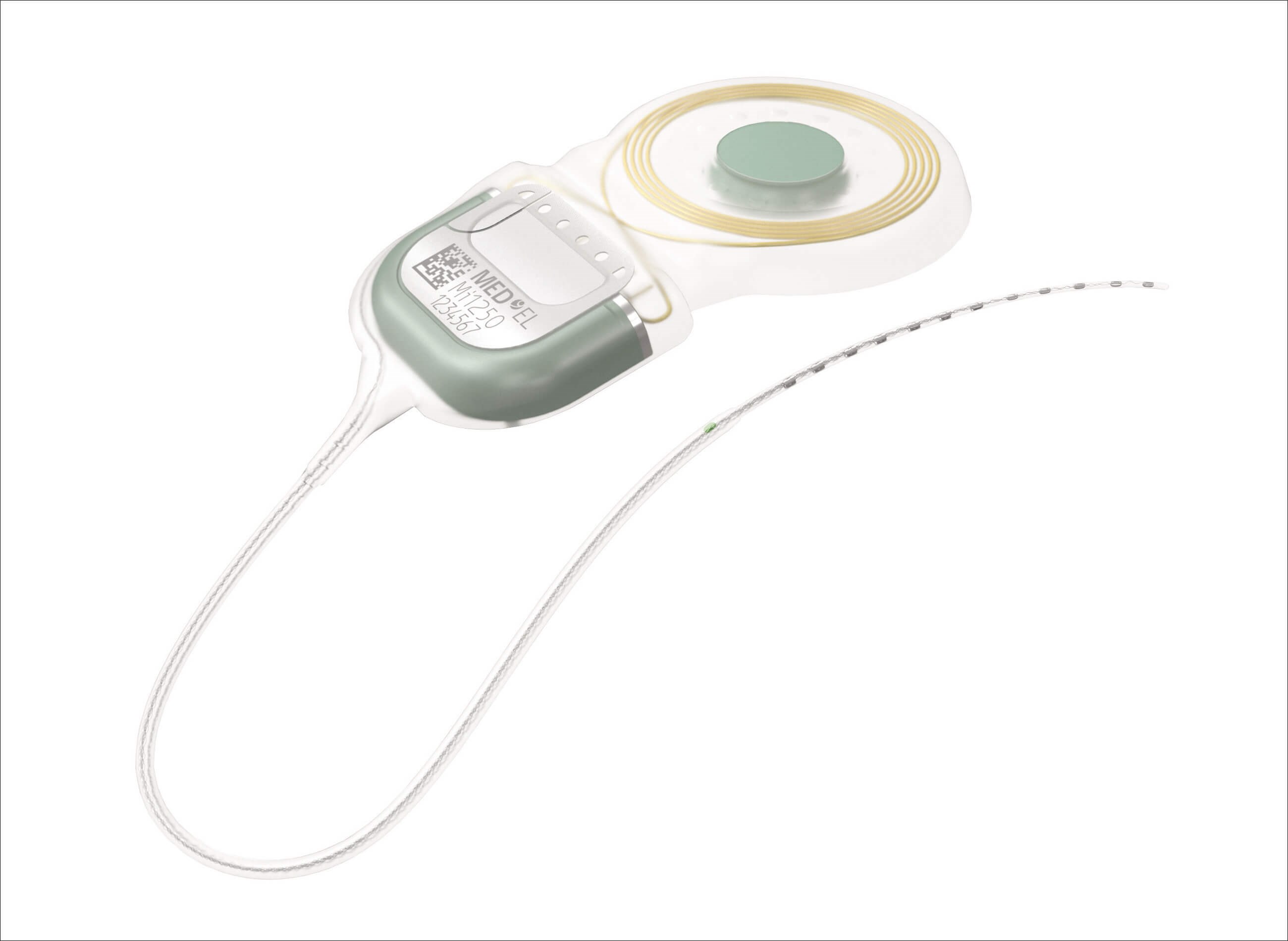
Image courtesy of MED-EL.
Paediatrics
Newborn hearing screening programmes, genetic testing and advanced imaging techniques have enabled significant progress in neonatal and paediatric cochlear implantation. Significantly, congenitally deaf children are now implanted around the age of 12 months, a practice that carries minimal risk and offers optimal outcomes by rehabilitating hearing well before the closure of the window of neuroplasticity, which diminishes rapidly after the age of ~3.5 years. Bilateral simultaneous implantation of children is now the norm, as opposed to sequential implantation in the past. The rehabilitation of hearing in babies and children brings new challenges in the form of lifelong follow-up and maintenance.
Rehabilitation and maximising outcomes
Rehabilitation – training and supporting patients to use their cochlear implant optimally – is essential. Stimulation of the auditory nerve alone does not impart a sense of useful hearing; the auditory cortex also needs to adapt. Emerging technologies aim to support improved outcomes, including anatomy-based fitting, which aligns electrical stimulation with the cochlea’s natural frequency map. However, the key to optimal rehabilitation is regular use of the activated implant, supported by professional input in the form of auditory-verbal therapy for children and rehabilitation support from specialists in the field. The support of family and social networks can also make a significant difference to patients learning to hear through their cochlear implant in a variety of environments.
A key development in rehabilitation is the use of telehealth and remote programming. This is supported by software available to patients and professionals, and facilitates accessible contact between recipients and professionals.
Future directions
The next significant steps in cochlear implantation are likely to involve AI-driven strategies and smart systems to optimise sound processing. Totally implantable devices are now available in the early stages of clinical use. They enable recipients to hear without an external component; however, they bring challenges such as internal battery life and internal microphone function. On a global scale, expansion of global access and cost-effectiveness of cochlear implants are important. Regenerative and genetics research have the potential to change the landscape of how severe to profound hearing losses are managed, significantly.
"Significantly, congenitally deaf children are now implanted around the age of 12 months, a practice that carries minimal risk and offers optimal outcomes by rehabilitating hearing well before the closure of the window of neuroplasticity"
Cochlear implants are one of the most successful neuroprostheses of all time, representing a significant intervention in the management of severe to profound hearing loss. As practice evolves, individualised care and an MDT-driven practice are essential for optimal decision-making, preoperative care, surgery and postoperative rehabilitation. New developments in the domains of genetic and regenerative medicine offer potential for the future but, for now, cochlear implants represent the gold standard intervention for children and adults with severe to profound hearing losses.
References
1. Cochlear implants for children and adults with severe to profound deafness, March 2019
https://www.nice.org.uk/guidance/ta566
[Link last accessed September 2025].
2. Cullington HE, Jiang D, Broomfield SJ. Cochlear implant services for children, young people and adults. Quality standard. Cochlear Implants Int 2023;24(sup1):S1–13.
Declaration of competing interests: None declared.
Emma Stapleton will present on this topic at the 20th ENT Masterclass® in January 2026.










