Paediatric airway emergencies are high-stakes, but training, simulation and updated guidelines help ENT teams manage risks and build confidence.
Congratulations to the ENT Masterclass® on its forthcoming 20th birthday. Over the past two decades, Shahed Quraishi has grown it to the international phenomenon that it is today. Paediatric otolaryngology has always been privileged to open the two-day proceedings of the annual UK meeting. In January, at the Royal Society of Medicine, it will again do so with an exploration of the challenges in paediatric airway management – in just 20 minutes!
We therefore usually concentrate on managing the acute paediatric airway rather than exploring subtle arguments of surgical technique. While there are few things more terrifying than airway obstruction in an infant, it is the responsibility of all ENT surgeons covering all ages of patients to be emergency-safe in the management of the paediatric airway. The paediatric airway session at the annual ENT Masterclass® is one of the regular opportunities for the trainees to be guided through the management and for more senior surgeons to be reminded of the available strategies.
We asked ChatGPT, which is only half the age of the ENT Masterclass®, what it thought the challenges in paediatric airway management were. This is broadly what it said:
- Well-known anatomical and physiological differences in children, which complicate management.
- Prediction of ‘difficult airways’ and anticipation of airway obstruction in children with congenital anomalies.
- Equipment, size and device limitations.
- Limited training and experience.
- Lack of standardised paediatric airway guidelines.
Understanding the anatomical and physiological characteristics of children which make airway compromise arise more quickly and dramatically than in adults, as well as recognising the signs indicating rapid escalation of airway compromise together with non-surgical measures to stabilise the situation, make it less scary. There are few clinical scenarios which are more stressful than a ‘can’t intubate, can’t ventilate’ situation. In the emergency situation, imaging has a limited role but antenatal imaging with foetal ultrasound and MRI has transformed the ability to identify congenital high airway obstruction and allow controlled delivery, such as by ex utero intrapartum treatment (EXIT).
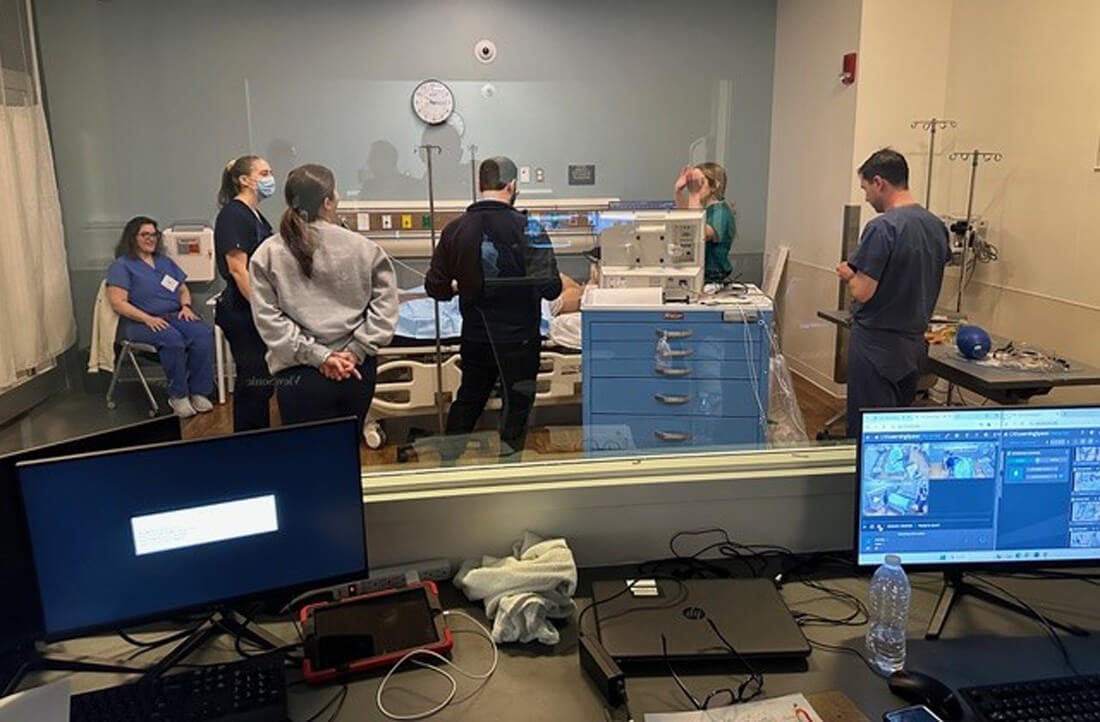
Team simulation of airway emergency management.

Practical bronchoscopy update for consultants, convened by BAPO.
It is the last three ‘challenges’ which have seen significant developments in the last 20 years. The development of videolaryngoscopes, such as the GlideScope, has reduced the incidence of failed intubation and, in more recent years, smaller videolaryngoscopes have become available as well as Mac and Miller (straight) blades for paediatric intubation. It would be important to ensure that these are available. Single-use flexible bronchoscopes are now also available down to 2.8 mm diameter, which can facilitate oral or nasal intubation. While THRIVE (transnasal humidified rapid insufflation ventilatory exchange) has shown the potential to extend apnoeic time, it has not been shown to improve the success rate of primary intubation. Equipment and drugs should be assembled in an airway trolley such as the MAST (Make Airways Safe Trolley) developed by the Southampton paediatric airway team.
"While there are few things more terrifying than airway obstruction in an infant, it is the responsibility of all ENT surgeons… to be emergency safe"
Limited training and experience in management of the acute paediatric airway is inevitable as the volume is low in relation to the number of ENT surgeons involved with their management. In the UK, it is no longer mandatory for an ENT trainee to rotate through a children’s hospital. It is therefore not infrequent that a trainee might not have carried out a paediatric tracheostomy by the time they achieve their CCT, and similarly, they may have had little or no experience with a ventilating bronchoscope. It is therefore essential for trainees and consultants to update their paediatric airway skills on simulation courses on a regular basis. Airway simulation, including tracheostomy, has been carried out with animals in the past. For bronchoscopy, this has been replaced by mannequins and for tracheostomy, it has been superseded by the evolution of 3D-printed neck models.
In the UK, The British Association for Paediatric Otolaryngology (BAPO) convenes the British Paediatric Airway Emergency Course (BPAEC) several times a year in different parts of the country. There is no established paediatric ENT simulation course in British Columbia, but the BC Children’s Hospital runs regular multidisciplinary airway scenarios in-house, as do other local hospitals. Queensland Children’s Hospital convenes a two-day formal paediatric airway course every year. Such courses attempt to bridge the experiential gap in the management of paediatric airway emergencies, not just by the ENT surgeon but by anaesthetists and nursing staff. Both British Columbia and Queensland are geographically huge areas where transfer of a child with airway obstruction in time may not be possible, and establishment and maintenance of local expertise needs to be done with regular simulation courses.
The Difficult Airway Society and the Association of Paediatric Anaesthetists have published excellent guidelines for managing the unanticipated difficult airway in children. These are written by anaesthetists and predominantly directed at a ‘difficult intubation’ scenario. The National Tracheostomy Safety Project has published well-researched and clear guidelines on the management of tracheostomy in children. Groups like IPOG (International Paediatric Otolaryngology Group) continue to develop consensus-based guidelines which include management of the acute paediatric airway.
So, ChatGPT was pretty accurate in framing the current challenges in paediatric airway management, but it missed ENT Masterclass® as a resource for updating and revising the knowledge base. Paediatric airway obstruction is an anxiety-provoking situation for the non-specialist paediatric ENT surgeon, and perhaps the biggest challenge is to put in place an infrastructure that reduces the surgeon’s anxiety and mitigates the risk to the child.
Declaration of competing interests: None declared.