Dr Alexander Simidchiev is a specialist in internal medicine, pulmonary medicine and public health. He is the Co-Founder and President of Air for Health, a non-profit organisation aimed at educating medical professionals about the impact of air pollution and climate change on human health. Here he discusses the importance of air pollution and climate change in rhinology.
Medical information is accumulating exponentially, with projected doubling time decreasing to some two months [1]. Air pollution and climate change are becoming important elements and required activities related to public health, but medical universities’ curricula are frequently lagging in integrating these topics, while continuing medical education is focused predominantly on clinical consequences rather than environmental causes. There is an increasing rift between clinical medicine and public health efforts, which requires efforts to realign these disciplines.
Air pollutants include toxic particulate matter and gaseous substances emitted in significant quantities from many combustible processes. They include particulate matter (PM), ozone, and biological contaminants, such as viruses and bacteria, which can penetrate the human airways and sometimes even reach the bloodstream, triggering airway inflammation, dysfunction, and fibrosis. PM varies in terms of composition and can include solid and liquid particles of various sizes. PM concentrations are usually higher in urbanised areas. In general, air pollution decreases quality of life and life expectancy via increasing chronic cardiovascular, respiratory, metabolic and malignant diseases. Pollutants that accumulate in the upper airways exacerbate symptoms of upper airway dysfunction and inflammatory diseases such as rhinitis, sinusitis, pharyngitis and laryngitis [2]. There is also data that air pollution increases the frequency and influences the outcomes of malignancy of the upper airways. The effects on the paediatric population add unfavourable consequences related to decreased speed of development in utero and postpartum.
Climate change affects both the environmental as well as social determinants of health [3]. The interaction between clean air and climate change, additionally decrease availability of safe drinking water, paucity of food supply and secure shelter and serve as a basis for social disruption. This will increase migration, epidemics, malnutrition, and regional conflicts. Apart from the ‘macro’ effects on populations, increased ambient temperatures and changes in humidity as well as concentration of population will impact on the upper airway microenvironment and, from there, will have effects on the microbiota [4] which will feed back to dysregulation of the local immune reactivity. The local immune response will be initiated, enhanced, and sustained by epithelial barrier dysfunction [5].
SEE ALSO
Particulate matter air pollution has been implicated in many disease states, but the results are frequently difficult to interpret between studies due to differing chemical composition of the particles, differing concentrations, exposure times, different populations, age composition and pre-existing medical conditions. The nose and upper airways are directly exposed as first-line organs to air pollution, and their aerodynamic characteristics define their role as ‘air-conditioners’ and ‘large-particle filters’. This means their concentration/disease response characteristics are more skewed towards larger aerosols (PM10) versus smaller aerosols (PM2.5, PM1.0, PM0.1) responsible for the multitude of chronic internal organ conditions (cardiovascular, respiratory, metabolic etc.). The particulate aerosols, when deposited on the mucosal surfaces of the upper airways, elicit inflammatory responses due to the chemical interactions that lead to a change in upper airway geometry/blood supply and inflammasome. These changes cause two distinct effects – barrier dysfunction and microbiome shifts/disruption. Both of these effects lead to a tendency towards chronicity, especially with persistent exposure to the causative air-pollution (see Figure 1 defining the distinctive characteristics of the upper vs. the lower airways and the related microbiota populations).
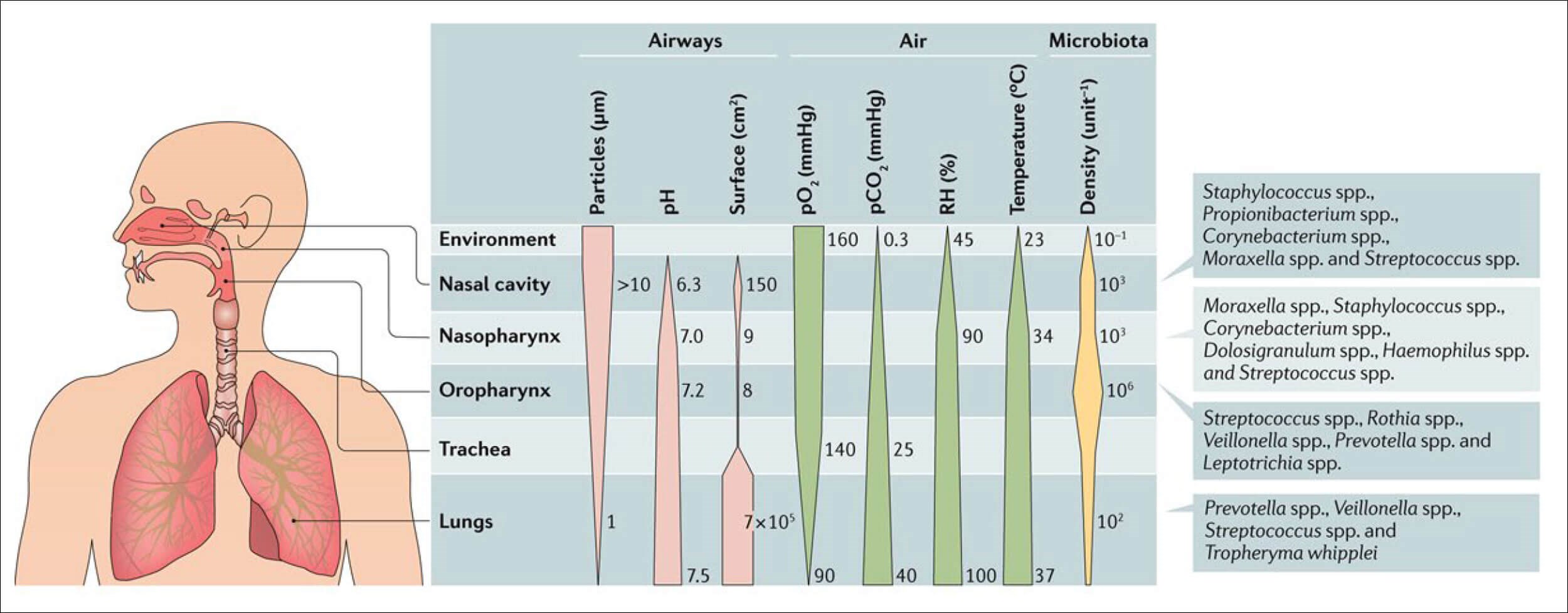
Figure. 1 Microenvironment and microbiota [4].
The intimate contact with pollutants and microbiota also causes the so-called epithelial barrier dysfunction [5], leading to a ‘leakiness’ augmenting the damaging effects of the pollutants and the microbiota microenvironment. Disruption of the zonula-occludens proteins as well as occludin and claudin leading to separation of the tight junctions allow facilitated transfers of ‘outside-in’ toxins as well as leakage of ‘inside-out’ inflammatory mediators.
Climate change is a slower but much harder to manage pathogenic process, as it is affected both by direct influences (temperature, humidity, pollution and infectious agents) as well as by social effects (migration, food-supply, behavioural changes, policies and political decisions). Climate change has important effects related to environmental pollution and the origin of hypersensitivity and pollen allergy. The education of the population and governmental decisions to prevent environmental pollution and climate change are urgent measures throughout the world. Adaptation and mitigation measures can be undertaken to limit climate change impacts on air pollution induced by chemical agents, pollens, and moulds.
Both climate change and air pollution are causally related anthropogenic effects on our environment. They change our living space in a way that causes an increased frequency of disease, increased healthcare expenditure, loss of quality of life and increased mortality. Public health efforts to improve adaptation to climate change and effective mitigation of air pollution at a population level, needs to be complemented by individual/patient-level efforts by clinicians. ENT specialists are well positioned to support this, provided they are well informed and given the tools to do this. This article is an attempt to lift a small corner of the curtain, share information and enable further efforts to increase awareness, promote advocacy and ultimately usher in the necessary change for our society.
References
1. Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2011;122:48-58.
2. Luo X, Hong H, Lu Y, et al. Impact of air pollution and meteorological factors on incidence of allergic rhinitis: A low-latitude multicity study in China. Allergy 2022, in press.
3. Joshi M, Goraya H, Joshi A, Bartter T. Climate change and respiratory diseases: a 2020 perspective. Curr Opin Pulm Med 2020;26(2):119-27.
4. Man WH, de Steenhuijsen Piters WAA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol 2017;15(5):259-70.
5. Sozener ZC, Ozturk BO, Cerciet P. Epithelial barrier hypothesis: Effect of the external exposome on the microbiome and epithelial barriers in allergic disease. Allergy 2022;77(5):1418-49.