Whilst the majority of patients with chronic rhinosinusitis (CRS) will significantly improve with treatment, we are sometimes left with a ‘hard-core’ of nasal cripples who fail to improve despite our best efforts. How can we deal with these patients? Valerie Lund and Wytske Fokkens give us their insight.
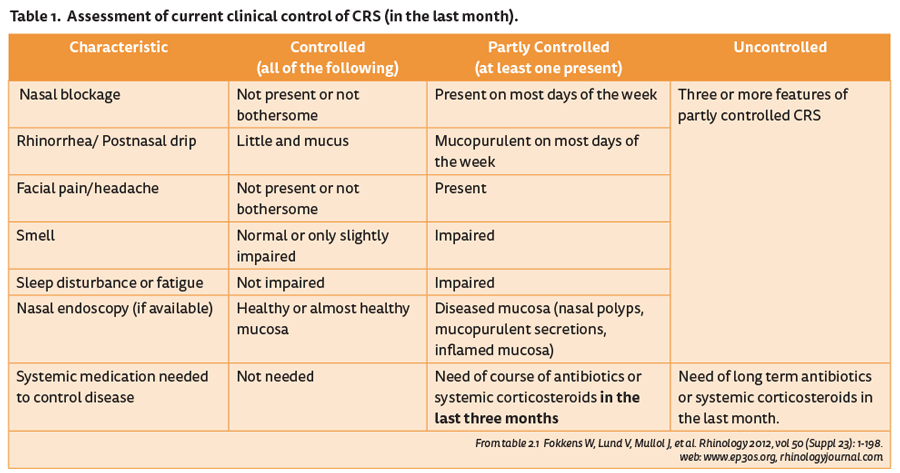
In the last iteration of EPOS [1], we introduced the term of ‘difficult-to-treat’ rhinosinusitis, defined as a patient who has persistent symptoms of rhinosinusitis despite appropriate treatment. This usually means a failure of symptom control despite adequate surgery, intranasal corticosteroid treatment and up to two short courses of antibiotics or systemic corticosteroids in the last year (Table 1).
The concept of control is one which is recognised in asthma and translates well to CRS, reinforcing the recognition of the unified airway. The reasons for lack of control can be considered in four main areas [2].
- Diagnosis-related factors, e.g. incorrect diagnosis, concomitant local and / or systemic disease
- Disease-related, e.g. exogenous / endogenous / genetic factors
- Treatment-related factors, e.g. inadequate treatment, lack of symptom-orientated treatment
- Patient-related factors, e.g. compliance.
The first question we should ask is, “Is it really CRS?” Patients for whom significant facial pain is the main or only symptom rarely have CRS, especially in those with nasal polyps. Similarly mucosal retention cysts are ‘incidentalomas’ and asymptomatic whilst any CT scan performed within 6-8 weeks of a common cold will continue to show mucosal thickening which is not clinically relevant .
It may be that the patient has undiagnosed asthma and / or aspirin-exacerbated respiratory disease (AERD), both of which adversely affect prognosis and can usually be recognised by history and confirmed by a few simple clinical tests. The cardinal features of Churg Strauss syndrome or eosinophilic granulomatosis with polyangitis (EGPA) are CRS with nasal polyposis (CRSwNP), asthma and systemic eosinophilia, which covers the demographic of many of our patients.
“The goal of treatment is to achieve and maintain clinical control. Control is defined as a disease state in which the patient does not have symptoms or the symptoms are not bothersome, if possible combined with a healthy or almost healthy mucosa and only the need for local medication.”
Although rare (~4 million per year in the UK), this diagnosis should be considered in any severely affected patient, otherwise it may be overlooked until other systemic problems such as cardiomyopathy and peripheral neuropathy occur. Unfortunately p-ANCA is only positive in around 50% of cases. Other granulomatoses such as GPA (granulomatosis with polyangitis / Wegener’s) and sarcoidosis may mimic severe CRS, having similar scores on outcome tests such as the SNOT22 as ‘ordinary’ CRS, and will require appropriate blood and tissue diagnoses.
Inherited conditions such as cystic fibrosis and primary ciliary dyskinesia should not be discounted in an adult with recalcitrant CRS and genetic and cilial tests (saccharine clearance, expired nitric oxide and electron microscopy) should be considered in suspicious cases. Similarly, subtle immune deficiencies are more common than is often realised with IgA and IgG subclass deficiencies being found in ~5-6% of patients with problematic CRS. Sometimes it can be an unsuspected anaemia, leukaemia, liver, renal or endocrine disturbance such as thyroid disease which presents as recalcitrant RS and is only revealed by a general haematology screen.
Addressing environmental issues such as smoking should be considered, as both active and passive smoking is associated with higher prevalence of CRS and poorer outcomes. Allergic rhinitis is known to increase the frequency and duration of upper respiratory tract infections. And we also have to deal with patient-related problems such as inflated expectation and poor compliance with medication use and advice. Of course as clinicians, our treatments may be inadequate, inappropriate or surgically overly ambitious or aggressive leading to stenosis, fibrosis and neo-osteogenesis which can be difficult to rectify.
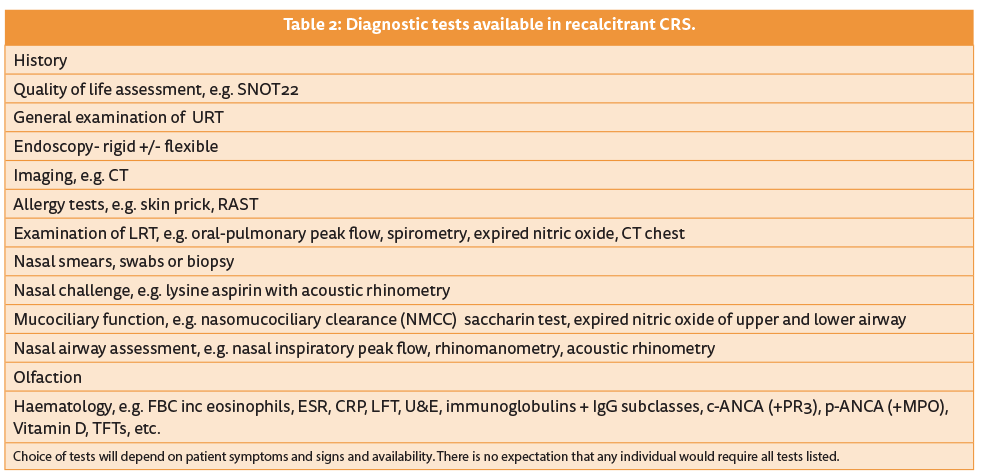
Diagnostic tests
We have many diagnostic tests at our disposal, although a thorough history and careful endoscopic examination remain the most important. A wide range of others can be undertaken in the recalcitrant case (Table 2), depending on the specific symptoms and signs [3]. Some are only available in specialist centres but most can be undertaken in any hospital and will at least screen for many of the conditions. However, even when some tests are negative, this may not exclude the diagnosis. For example c-ANCA is only 47% specific in limited GPA when confined to the upper respiratory tract and where it often starts, as compared to systemic disease (81% specific), and in 10% p-ANCA can be positive.
Consequently, we would recommend in the really resistant cases of CRS to ‘share the pain and phone a friend’, be it another ENT colleague, specialist rhinologist or physician, allergist, immunologist, pneumatologist or rheumatologist. Or better still, find a physician with an interest in the nose and run a combined clinic. We have been involved in a specialist rhinology clinic for over 30 years with colleagues whose backgrounds have been allergy, immunology and respiratory and we cannot recommend it too highly, both for the patients and clinicians involved. Complex cases involving the entire respiratory tract and beyond require a holistic approach and the relationship is symbiotic for all concerned.
Treatment
If any of the systemic conditions are confirmed, specific systemic treatment regimes will be employed, ranging from nebulised antibiotics and genetic modulators such as ivacaftor in cystic fibrosis, prednisolone, steroid-sparing cytotoxic agents and monoclonal antibodies, e.g. rituximab in the vasculitides, to immune replacement therapy in the immunodeficient. These in turn may improve the nasal problems although nasal douching and topical intranasal steroids and lubricants usually continue to be employed.
“We have been involved in a specialist rhinology clinic for over 30 years with colleagues whose backgrounds have been allergy, immunology and respiratory medicine and we cannot recommend it too highly, both for the patient and clinicians involved.”
The nasal symptoms and recurrence of nasal polyps associated with AERD have now been shown in at least two randomised controlled trials (RCTs) to be improved by aspirin desensitisation but this must be undertaken with considerable care.
However, frequently no contributory condition is identified and we are left with a distressed patient seeking more extreme forms of treatment gleaned from the internet or wondering if their twentieth polypectomy will work any better than the previous ones. Further surgery may indeed continue to play a role, more often in CRSwNP than CRS without (CRSsNP), but it is important to manage patient expectation as to what it may achieve and for how long. In fact, education and psychological support should be considered as significant components of our management.
Perhaps we should take an alternative view of this problem and consider more carefully how we treat patients from the outset, once we are confident of the diagnosis. Certainly the concept of personalised or precision medicine is the hot topic across medicine [4]. Traditionally we have tended to throw everything we can at the problem – steroid sprays / drops / tablets, douching, antibiotics and surgery - without considering the heterogeneity of CRS. It is generally accepted that CRSwNP has a different phenotype from CRSsNP but perhaps we should be unpicking this further as has recently been possible with the GALEN cohort, in which more than 17 endotypes were identified by cluster analysis [5].
If we were able to more precisely direct our treatments based on markers such as eosinophil numbers in blood or nasal mucus and / or levels of IgE, IL4 or IL5, we might anticipate better responses and reduce the progression of disease with its associated remodelling of mucosa and adjacent bone (Figure 1). However, the expense of the new biologics will need to be set against the potential savings from fewer operations, and initially their main role may be in the recalcitrant cases only.
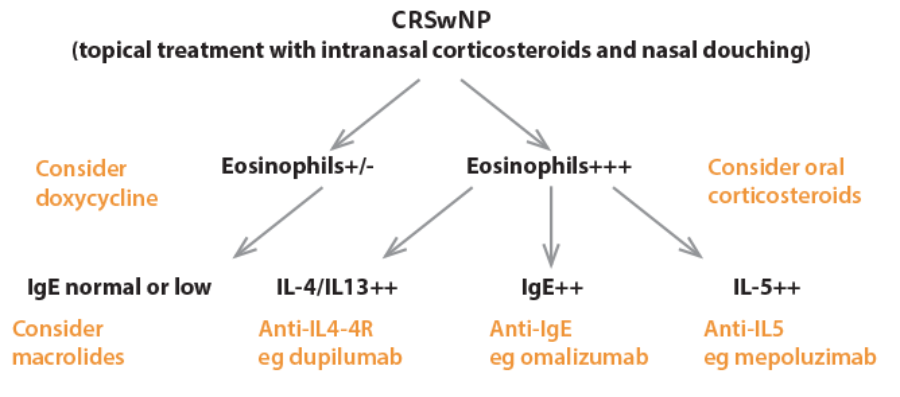
Figure 1. ‘Precision medicine’. Possible theraeutic approach based on endotypes of disease in CRSwNP.
Despite the somewhat unpredictable natural history of sinonasal inflammation, we are all generally agreed on a reasonable period of ‘optimal’ medical treatment, whatever that may be. However, there is some evidence that when this fails, we should not delay surgery too long [6]. Operating within one year of the onset of CRS symptoms appeared to produce significantly better outcomes as judged by SNOT22 scores compared to patients in whom surgery was undertaken much later. To paraphrase that rather over-worked adage, “Prevention of recalcitrant rhinosinusitis will almost certainly be better than trying to cure it”.
SUMMARY
In recalcitrant chronic rhinosinusitis:
-
Consider if it is really CRS?
-
Consider other respiratory disease, e.g. asthma, AERD
-
Consider other systemic conditions, e.g. vasculitis, immune deficiency, cystic fibrosis, primary ciliary dyskinesia – if you don’t think of them, you won’t diagnose them!
-
Share the problem – manage collaboratively with physicians.
References
1. Fokkens W, Lund V, Mullol J, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinology 2012;50(S23):1-198.
2. Hellings P, Fokkens W, Akdis C, et al. Uncontrolled allergic rhinitis and chronic rhinosinusitis: where do we stand today? Allergy 2013;68:1-7.
3. Scadding G, Hellings P, Alobid I, et al. Executive Summary of European Task Force on Diagnostic tools in Rhinology. Rhinology 2012;50:339-52.
4. Muraro A, Fokkens W, Pietikainen S, et al. European symposium on precision medicine in allergy and airways diseases: report of the European Union parliament symposium (October 14, 2015). Rhinology 2015;54:303-7.
5. Tomassen P, Vandeplas G, Van Zele T, et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clinical Immunology 2016;137(5):1449-56.
6. Hopkins C, Rimmer J, Lund V. Does time to endoscopic sinus surgery impact outcomes in Chronic Rhinosinusitis? Prospective findings from the National Comparative Audit of Surgery for Nasal Polyposis and Chronic Rhinosinusitis? Rhinology 2015;53:10-17.
Declaration of Competing Interests: None declared.





