A new diagnostic test that is quick and has directly applicable results to hearing aid settings has arrived, but how does it work? Leigh Martin has the answers.
In an earlier article for ENT & Audiology News, Parmar and Rajasingam reported several barriers preventing many clinicians from performing speech-in-noise testing routinely in clinic [1]. These include access to appropriate speech materials, test time, and a lack of normative data.
Despite these challenges, audiologists accepted that these tests provide a huge amount of information to clinicians. It is therefore important for our profession to continuously look to develop clinically friendly ways to collect this information.
The Audible Contrast Threshold test, or ACT™, is a newly developed test designed to overcome many of the challenges associated with speech-in-noise testing. Firstly, it is based on the psychoacoustic principles of spectro-temporal modulation (STM), meaning it is language independent and therefore can be performed on anyone regardless of language background and ability. Secondly, the test can be performed quickly in less than two minutes using the same equipment as audiometry: a set of headphones, or insert earphones, and a push button. Lastly, ACT has a normative dataset which allows audiologists to gain an understanding of how their patients’ aided hearing-in-noise ability compares with a normally hearing population. The ACT value can then be used to automatically or manually adjust the advanced help-in-noise settings in the hearing aids, giving further clinical applications beyond traditional speech testing.
ACT is based on spectro-temporal modulation
Chi et al were the first to start work in this area developing a spectro-temporally modulated stimulus which, in certain configurations, shares important features with speech [2]. The stimulus consisted of a noise carrier which was modulated both spectrally and temporally using a moving ripple pattern. In other words, it sounds like a noise burst containing a siren and, most importantly, contains a structure similar to the modulations found in real speech. By changing the amount of modulation in the signal, it is possible to record a result called a spectro-temporal modulation detection threshold.
"Part of the ACT implementation was to develop a new dB scale to allow clinicians to differentiate between signals with differing amounts of modulation"
This generated excitement in the research community and, in the early 2010s, research articles began to appear in the literature showing high correlations between measures of speech-in-noise performance and spectro-temporal modulation (STM) detection thresholds in participants with hearing loss [3,4]. However, these early implementations of spectro-temporal modulation tests were limited, and it was not possible to perform this test clinically. It would take a further 10 years of research development before the principles of spectro-temporal modulation could be turned into the clinical test we call ACT today [5].
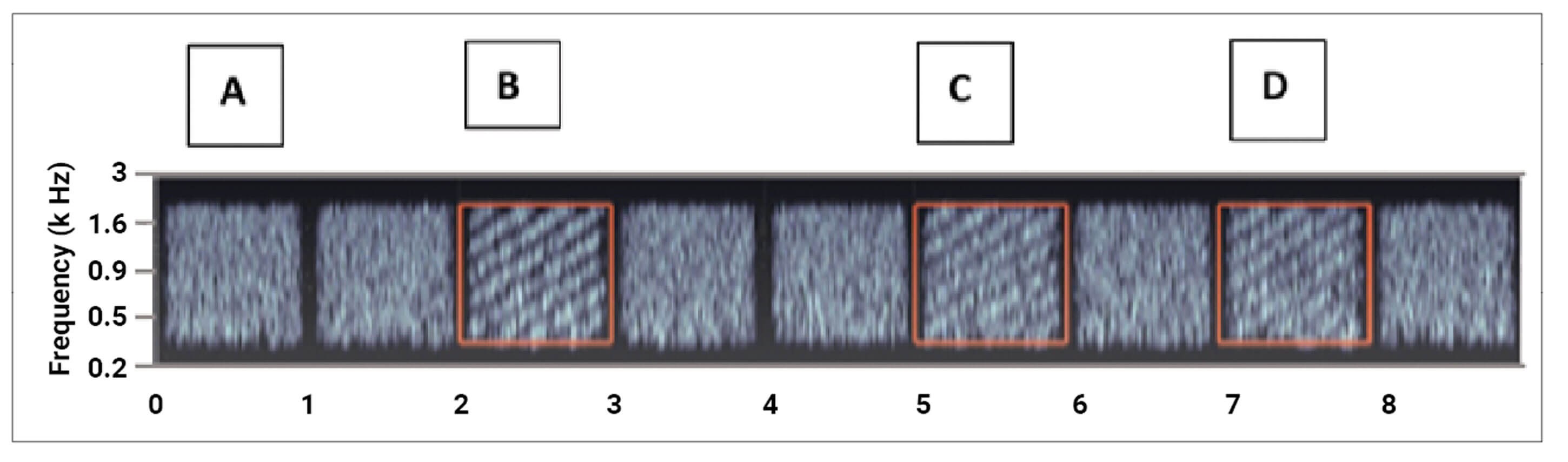
Figure 1: Illustration of the waves test paradigm used with ACT in spectrogram format.
The modulated target waves are indicated with red boxes in the spectrogram.
The ACT test
Today, the clinical version of STM detection is the ACT test. It works by continuously presenting bursts of noise to the patient (A in Figure 1). On occasions, a modulated noise signal is presented to the patient by the audiologist (B in Figure 1). This sounds like a siren on top of the noise. If the siren is detected by the patient, the amount of modulation in the signal is then reduced (C in Figure 1). Instead of looking at a visual representation of the stimulus, as seen in Figure 1, part of the ACT implementation was to develop a new dB scale to allow clinicians to differentiate between signals with differing amounts of modulation. This is called the dB nCL (decibels normalised contrast level) scale. When the dB nCL is high, the siren is easier to hear as there is a high amount of modulation (A in Figure 1). When the dB nCL is low, the siren is more difficult to distinguish from the noise as the modulation is less (D in Figure 1).
Running an ACT test
The starting level of the test, regardless of speech-in-noise ability, is the maximum contrast of 16 dB nCL. The audiologist presents this stimulus and, if the patient can detect the siren within the signal, they then press the response button. Using a similar ascending/descending technique as used in audiometry, the audiologist then reduces the amount of modulation in the stimulus in 4 dB nCL steps until the patient cannot differentiate the modulated signal from the noise-only signal. After that, modulation is increased in steps of 2 dB nCL and so on. Threshold is defined when three out of five ascending points are obtained at the same modulation level.
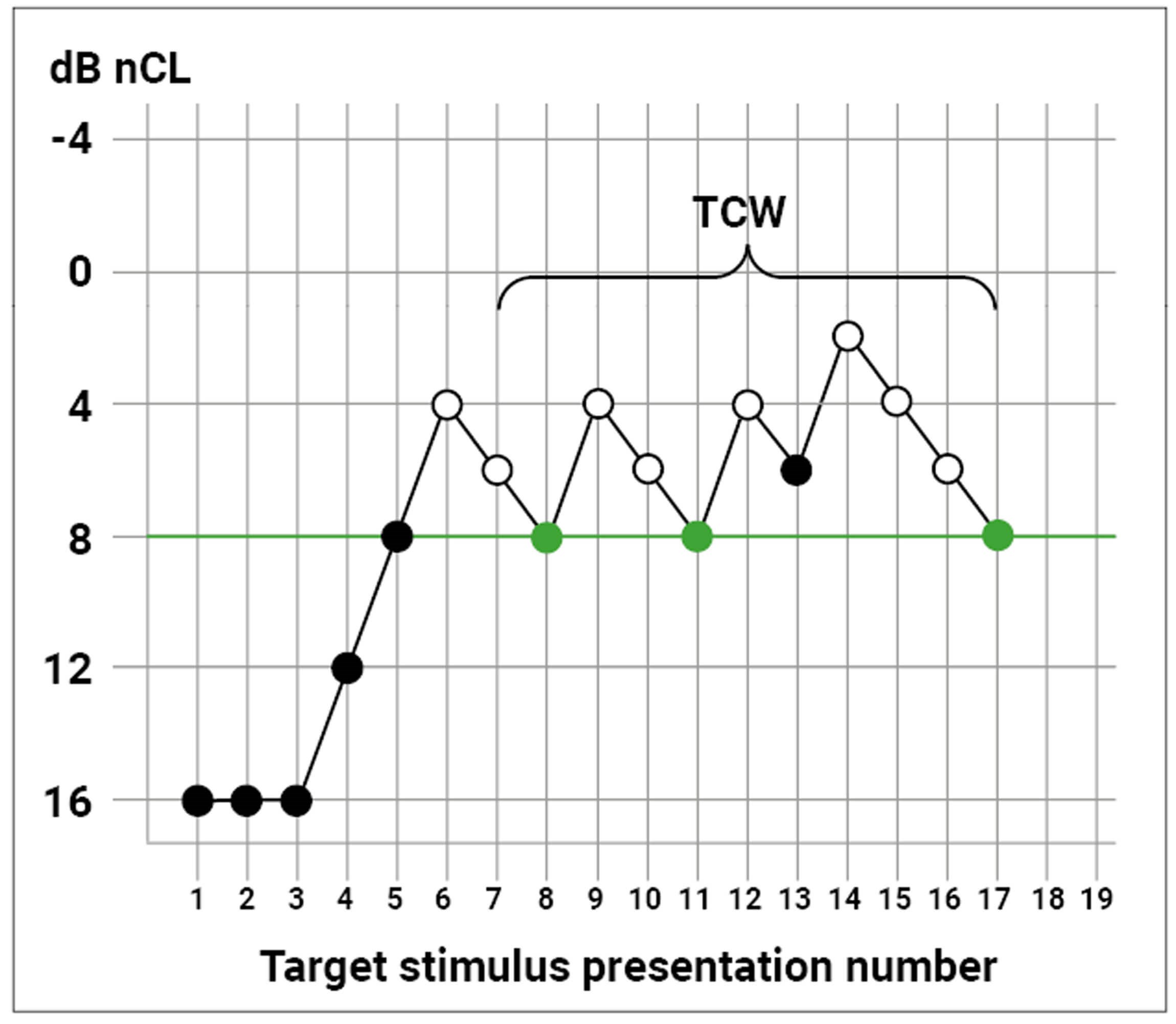
Figure 2: Example ‘tracking trace’ of an ACT run.
A filled symbol indicates a target stimulus presentation correctly detected
by the test participant; an open symbol indicates a target that was not detected.
To explain this further, Figure 2 shows an example of the steps required to generate an ACT value. The x-axis shows stimulus presentations, and the y-axis shows the level of modulation in the signal expressed in dB nCL. In this instance, the audiologist familiarised the patient with the test by presenting three signals at 16 dB nCL. The patient correctly responded to the signal as indicated by a black circle. The audiologist then began to reduce the dB nCL level in 4 dB nCL steps until the patient could not detect the siren within the signal. This is noted by the first unfilled circle at trial five. The next stage of the test is to increase the amount of modulation level in 2 dB nCL steps until the patient detects the modulation again. The process of decreasing and increasing the dB nCL level is then repeated until three ascending modulations are heard. So, in this example the threshold is at 8 dB nCL.
Interpreting the ACT test
The threshold measured by the ACT test is referred to as the ACT value. The ACT value will range from -4 dB nCL to 16 dB nCL. It can be used to inform the hearing care professional of how well a person with hearing loss will hear speech in background noise when wearing hearing aids. The lower the ACT value, the better the patient will be able to hear speech in noise. The higher the ACT value, the more difficulty they will have hearing when in background noise.
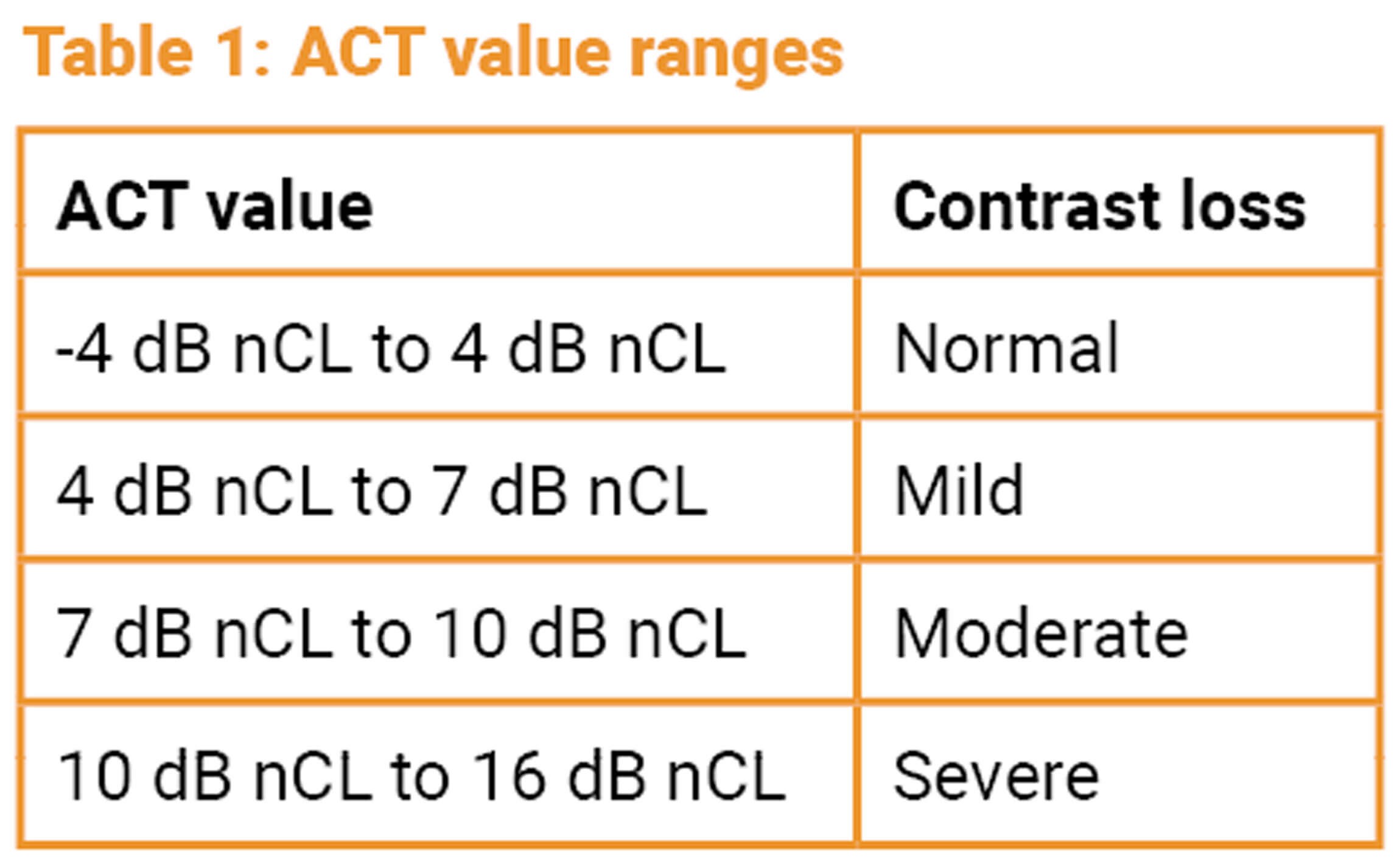
The Interacoustics Research Unit has identified ranges for the ACT value measured in the ACT test (Table 1).
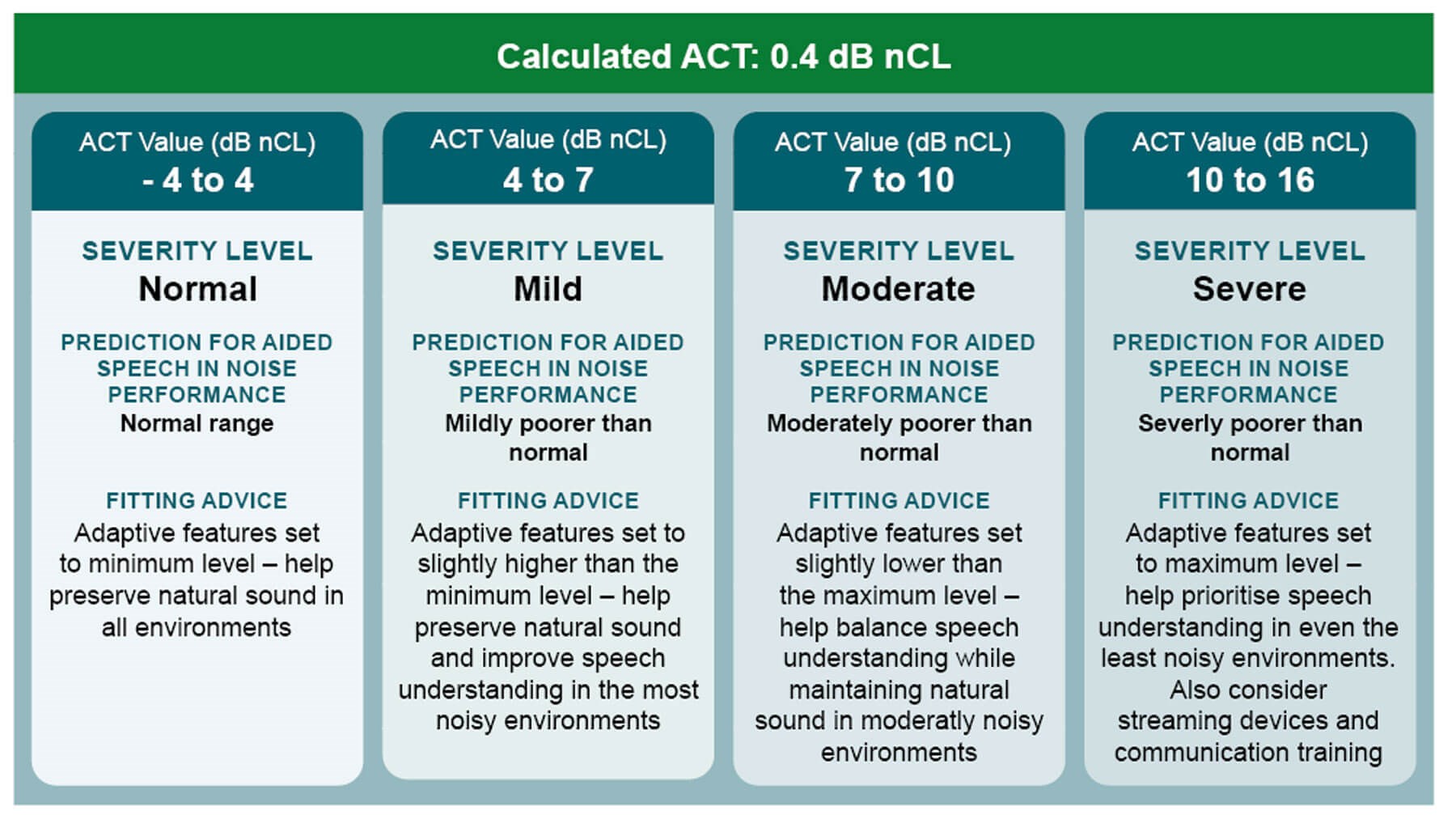
Figure 3: Fitting advice based on ACT value.
Further to the table above, a counselling tool has also been developed to provide clinicians with guidance on how to use the ACT value in clinical practice (Figure 3). To take an example, if someone has an ACT value of 14 dB nCL, then this indicates a severe contrast loss which means that the patient is expected to have severe challenges hearing in noise. This patient will therefore require the maximum help from the help-in-noise settings on their hearing aids (such as directionality and noise reduction) and their hearing aids should be programmed accordingly. In addition to this counselling tool, we are also now seeing individual hearing aid manufacturers being able to directly input the ACT value into the hearing aid fitting software which will cause automatic programming of the advanced hearing aid features based on their hearing-in-noise performance, as measured by the ACT test.
"The ACT value can be used to automatically programme advanced hearing aid features"
In summary, the ACT test is a language-independent test which predicts aided speech-in-noise ability and can be performed using an audiometer in less than two minutes. The result: the ACT value can be used to automatically programme advanced hearing aid features. By breaking down the barriers associated with traditional speech testing, it is hoped that ACT can be used in clinics across the world to improve the hearing aid outcomes of patients with hearing loss.
References
1. Parmar B, Rajasingam S. Adult speech testing in the UK. ENT & Audiology News 2023;32(2):32–4.
2. Chi T, Gao Y, Guyton MC, et al. Spectro-temporal modulation transfer functions and speech intelligibility. J Acoust Soc Am 1999;106(5):2719–32.
3. Bernstein J, Mehraei G, Shamma S, et al. Spectrotemporal modulation sensitivity as a predictor of speech intelligibility for hearing-impaired listeners. J. Am. Acad. Audiol 2013;124(4):293–306.
4. Mehraei G, Gallun J, Leek MR, et al. Spectro-temporal modulation sensitivity for hearing-impaired listeners: Dependence on carrier center frequency and the relationship to speech intelligibility. J Acoust Soc Am 2014;136(1):301–16.
5. Zaar J, Simonsen L, Dau T, Laugesen S. Toward a clinically viable spectro-temporal modulation test for predicting supra-threshold speech reception in hearing-impaired listeners. Hear Res 2023;427:108650.
Declaration of competing interests: LM is employed by Interacoustics A/S as Director of the Interacoustics Academy.








