The evolution of bone-conduction hearing devices from the 1400s’ rudimentary designs to today’s advanced models has greatly improved hearing for individuals with conductive or mixed hearing loss. This article delves into the history and technical advancements over the years, as well as shedding light on the challenges and choices faced by users and clinicians.
The history of bone-conduction hearing and bone-conduction hearing devices (BCDs) goes back to the 1400s and has been described in great detail by Murdy and Tjellström [1]. Most likely, the Italian physician G Cardano developed the first BCD. He used a rod placed between someone’s teeth, attached to a musical instrument, enabling a subject with hearing loss to hear the music.
Later on, a similar rod was connected to a kind of horn into which a speaker had to talk. That application was not very successful. Major steps forward took place during the technological revolution, in the early 1900s. In 1933, an electronic BCD was developed with microphone, amplifier and an actuator (vibrator), to be placed on the mastoid, kept in place by a steel headband. Owing to miniaturisation, in the mid-1950s, BCDs were fixed into the arms of eyeglasses, replacing the headband [1]. All these devices are referred to as ‘conventional BCDs’.
A BCD needs a powerful amplifier to stimulate the cochlea, as bone conduction is not efficient. Hearing thresholds, obtained with a standard bone-conduction actuator connected to a hearing device, were approximately 50 dB worse than when that device was coupled to the ear with an earphone. Furthermore, the efficiency of BCDs depends on the (acquired) pressure with which the actuator is pressed against the skin, which might lead to skin problems [2,3].
"He used a rod placed between someone’s teeth, attached to a musical instrument, enabling a subject with hearing loss to hear the music"
The skin and tissue layers between the actuator and the skull contribute to the inefficiency of BCDs as they attenuate the vibrations considerably [1,2]. Tjellström and Håkansson had the idea to bypass the skin and tissue layers using a skin-penetrating titanium implant, anchored in the mastoid bone, referred to as the percutaneous BCD (or pBCD) [1,2]. A specially developed audio processor was coupled to the implant (creating the ‘Baha device’). Measurements showed improved gain in the order of 10‑15 dB [2].
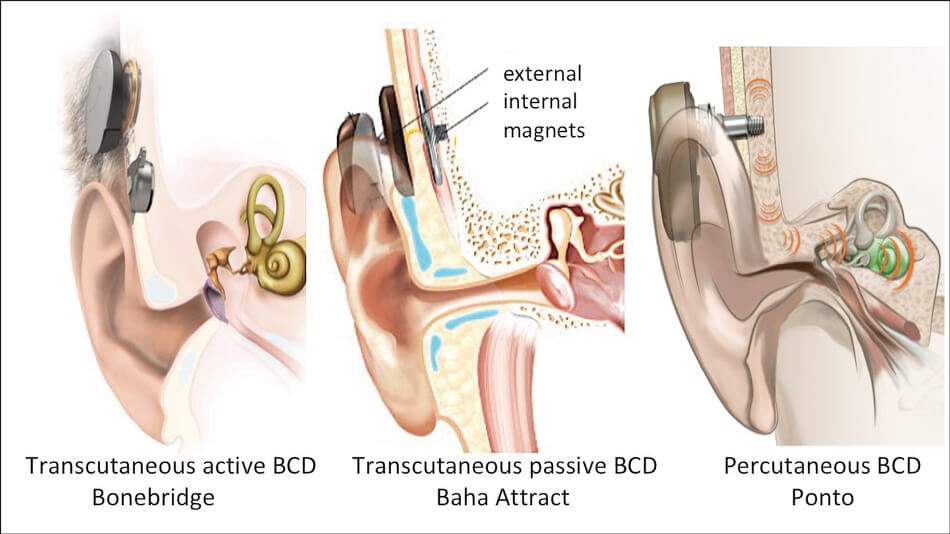
Figure 1. Examples of three different types of BCD. Images provided by Oticon Medical, Askim,
Sweden; Cochlear BAS, Gothenburg, Sweden and Med-El, Innsbruck, Austria, respectively.
These pBCDs (see Figure 1) have been on the market now for more than 40 years. During these years, the BCDs have been updated regularly and, besides the standard audio processor, more powerful processors have been developed. Nowadays, the Baha device (Cochlear BAS, Gothenburg, Sweden) and the Ponto device (Oticon Medical, Askim, Denmark) are available.
The thickness of a patient’s skull can be an issue; implantation of the titanium implant in children is only possible from three to four years onwards [3]. For younger children who need a BCD, the (also updated) conventional solution remains. To keep the actuator in place, a so-called softband was introduced in 2002, which is better tolerated by children [3]. In 2012/2014, BCDs with a magnetic coupling were marketed (see Figure 1). For this purpose, a magnet has to be placed subcutaneously, thus surgery is involved. Available now are the Sophono device (Medtronic, Dublin, Ireland) and the Baha Attract (Cochlear). In 2017, a BCD with an adhesive coupling was introduced; the Adhear device (Med-El, Innsbruck, Austria). Evidently, using transcutaneous transmission implies that these updated conventional BCDs are less powerful than pBCDs [3, Ch. 2.3, 3]. The devices with adhesive and magnetic coupling have not been developed specifically for children, but as an alternative for pBCD, to deal with skin problems that may occur around the percutaneous implant. Such problems are not rare [2], however complications leading to implant loss or revision surgery are rare. Long-term evaluation in adults showed one revision surgery per 43 years of follow up [3, Ch. 5.1.2]. Complication rates are approximately three times higher in children.
In 2012, a new, more powerful transcutaneous device was introduced: the Bonebridge (Med-El, see Figure 1), referred to as an ‘active transcutaneous BCD’. The actuator is implanted in the mastoid, under the skin, connected to an externally worn audio processor by a transmission link. First analyses showed that this device has an output that is largely comparable to that of a pBCD with standard audio processor [3, Ch.2.3]. In 2020, a similar type of BCD named the Osia device was released (Cochlear BAS) and Oticon Medical has developed an active transcutaneous device, the Sentio, to be launched in 2024.
"Counselling is of utmost importance"
It is unknown how often these different types of BCDs are applied. As an indirect indicator, we used the number of recently published papers per year between 2018 and 2022, using PubMed. For pBCD, although on the market for 40 years, a rather stable number of 30 per year was found, and for the updated conventional BCDs (with softband, adhesive or magnetic coupling) this number was also stable: 10. For the transcutaneous active BCDs, an increase was seen from 15 to 25 per year. This data should be considered with caution, as the number of publications doesn’t reflect the success rates of these devices, only the number of experimental and clinical studies.
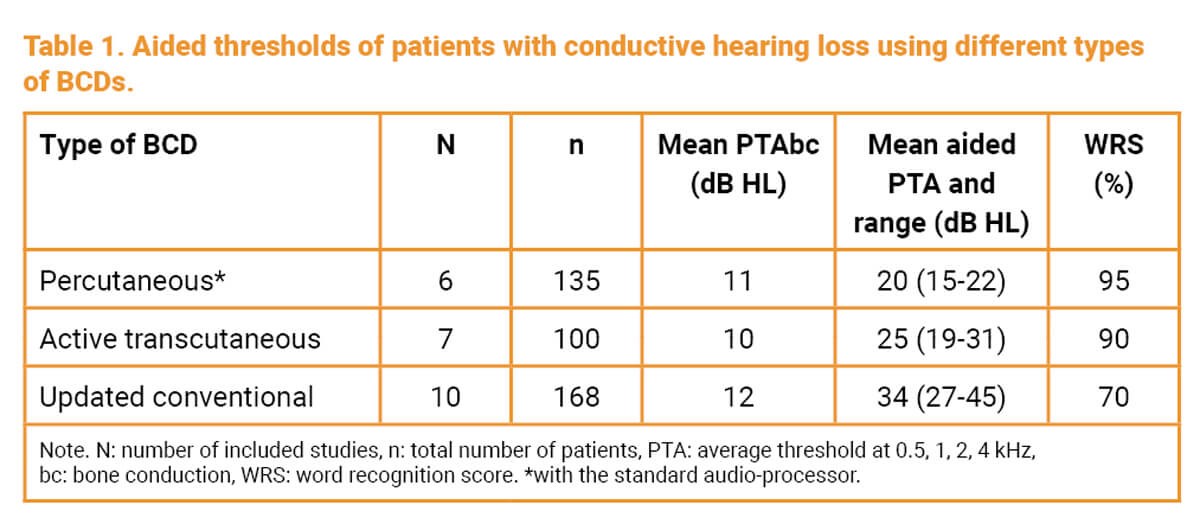
To compare the efficiency of the different types of BCD, a focused literature search was carried out, period 2010–2021 [3, Ch. 7.2.1]. Papers presenting aided thresholds of subjects with pure conductive hearing loss (cochlear thresholds < 20 dB HL) were selected. An overview of the data is presented in Table 1. Using the speech intelligibility index (SII) [3, Ch. 7.1] word scores were calculated; presented in the table. Clearly, the devices are not equivalents.
Thanks to the inventors and the companies, we have better options available to help patients with a conductive or mixed hearing loss. Choosing the best device for a patient is a challenge, especially for children developing speech and language. Given the level of efficiency and the limitations of the different options, taking into account the availability of more powerful audio processors to deal with ageing, counselling is of utmost importance. Aftercare should be discussed as well. A major step forward regarding counselling is the recent publication of consensus statements developed by clinicians and representatives of the manufacturers, aiming at shared decision making [4].
References
1. Mudry A, Tjellstrom A. Historical background of bone conduction hearing devices and bone conduction hearing aids. Adv Otorhinolaryngol 2011;71:1-9.
2. Tjellström A, Håkansson B. The bone-anchored hearing aid. Design principles, indications, and long-term clinical results. Otolaryngol Clin North Am 1995;28(1):53-72.
3. Snik A. Auditory Implants; Where do we stand at present? 2014.
www.snikimplants.nl
Last accessed September 2023.
4. Maier H, Lenarz T, Mir-Salim P, et al. Consensus Statement on Bone Conduction Devices and Active Middle Ear Implants in Conductive and Mixed Hearing Loss. Otol Neurotol 2022;43(5):513-29.










