Like Eeyore in AA Milne’s Winnie the Pooh stories it appears we all will soon have a personal cloud, but unlike Eeyore this will be something to celebrate! The future of hearing aid technology is in the cloud argues Uwe Andreas Hermann from the Eriksholm Research Centre, but not only will it contain our hearing aid data but essential biostatistics could be incorporated too; if it all sounds a little more George Orwell than Winnie the Pooh read on!
Today, the accepted consensus is that eHealth is coming to all forms of healthcare, including hearing healthcare, and that it will have a huge impact for users of hearing instruments and for hearing healthcare practitioners. Following the economic Kondratiev Model (Figure 1), eHealth will be part of the sixth big economic wave in the industrialisation process of mankind.
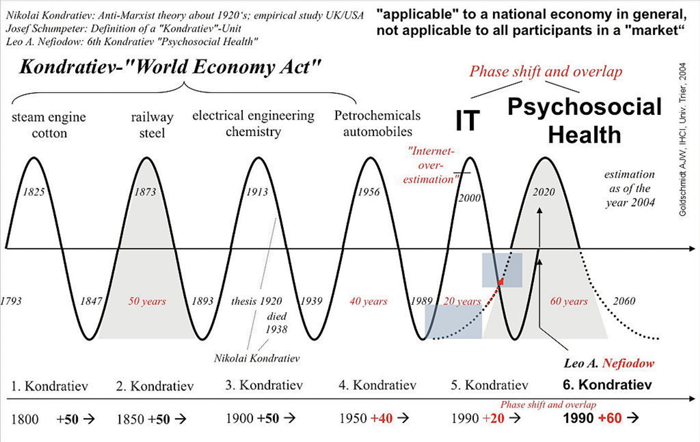
Figure 1: The economic Kondratiev Model. Wikipedia, Picture rights: CC BY-SA 3.0
Global players like Google, Microsoft, and IBM are exploiting their chances and launching pilot projects. But what exactly will eHealth mean for the hearing healthcare industry and for hearing aids of the future? To answer this, I would like to suggest a hypothetical journey into the future of a typical hearing instrument (HI) user.
“eHealth will be part of the sixth big economic wave in the industrialisation process of mankind.”
Hearing instruments will be permanently connected to a “cloud clinic” via a radio connection to the smartphone. So for example a user who is particularly happy with the performance of his HI in a given situation may signal this by pressing a “smiley” button of the HI app on his smartphone. In the opposite case, when the user is experiencing a difficult or even dissatisfying listening situation, he may press the “dislike” button instead. In such a case, the HI app will contact the cloud clinic and check whether there are alternative HI settings available, which gave a better listening experience to other, similar users. If such a potentially better setting is available for this particular sound environment, it will be downloaded and offered for immediate testing.
If the user still feels uncomfortable in a given sound environment, he may send a sound sample to his audiologist, which enables the expert to have a closer look at the related fitting parameters and download an update to the HI.
So in essence, the future HI user will never again need to feel alone with a hearing problem or challenging situation. Via the connectivity and remote service functions of the hearing instrument, he will be able to get instant help whenever and wherever.
“Instead of inventing apps and gadgets for which suitable problems have to be found, we have to work the other way around. We have to identify patient needs and develop solutions for them.”
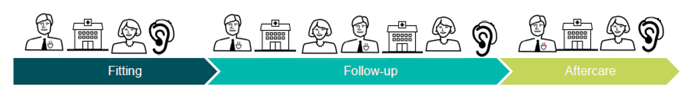
Figure 2: Client journey today (top) and Client journey tomorrow (bottom).
The eHealth services of the future will go far beyond this example and include aspects of personalisation, context awareness (like where is the HI being used in a given moment) and rehabilitation. We will have a whole range of new functions and services, of which we are only seeing the very beginnings today. However, some general aspects of future eHealth applications can already be clearly identified. eHealth will be:
- Omnipresent. You will not need to be sick in order to use it. Everybody will use it and it will have a global reach.
- “Always on”. Global connectivity will allow advanced IT systems (Big Data, Machine Learning) to provide individualised healthcare.
- Serving many purposes. It will improve quality of life, prolong independent living for the elderly and provide better services at lower costs.
eHealth is a rising Kondratiev wave today and its success in hearing healthcare will be determined by the following seven major factors:
- “People first”: Many eHealth projects are technology driven, but in reality technology is not the limiting element any longer. On the contrary, technology allows almost any thinkable solution, so it is about making the right choices for the benefit of our patients. Instead of inventing apps and gadgets for which suitable problems have to be found, we have to work the other way around. We have to identify patient needs and develop solutions for them.
- It is all about the “Patient journey”: We have to understand the patient journey starting from the very first moment when a patient is becoming aware that she / he has a hearing problem, through first contact with the health care provider, diagnosis, treatment, aftercare and to rehabilitation. Typically this is a long and complicated journey with problems, pitfalls, varying costs etc. When this is well understood, then we have to “invent” the appropriate, innovative eHealth solutions to improve this patient journey (Figure 2).
- Provider quality and care context: users are expecting individualised information, guidance and motivation corresponding to their particular situation, health problem and health literacy, not an automatic answering machine or an email auto response.
- Think about the patient holistically: Audiological patients often also suffer from co-morbidities. For example, elderly patients might have cardio vascular diseases, diabetes, dementia, risk of stroke, etc. These diseases obviously cannot be treated by an audiologist, but the audiologist can work closely together with other health care professionals to supply holistic solutions. Imagine if you could have hearing instruments in future which could be multi-sensory devices, containing measurements for temperature, pulse, EEG, acceleration, etc. (Figure 3). Suddenly the audiologist could become a provider of health monitoring data for a general practitioner, cardiologist or geriatric specialist.
- Think about the system holistically: The incompatibilities of today’s healthcare systems must be overcome, for example, often data has to be entered manually into patient records because diagnostic instruments lack compatible IT interfaces.
- Standardisation, preferably on a global level, will be the way forward, but this will not come easily. Typically it has to be driven by the users and their needs. In the 1980s the GSM mobile radio standard was driven by the European telecom operators who were tired of incompatible and expensive national standards.
- “eHealth is the use of information and communication technologies (ICT) for health..., eHealth is about improving the flow of information, through electronic means, to support the delivery of health services and the management of health systems.” (World Health Organization, 2012.) It is all about information, communication technologies and IT security. We will have to invent eHealth solutions which give trust and security to our patients. Their personal data must not be compromised on the global web.

Figure 3: Research version of a hearing aid with built-in EEG function.
Summing up and looking back at the Kondratiev wave I discussed at the beginning of this article, we may conclude that eHealth is a rising wave in healthcare, particularly hearing healthcare. We are already able to see the prospects of the future; eHealth will be big and will change our healthcare systems, but fundamentally, we must always focus on our patients and their needs.
Declaration of Competing Interests: The author is employed by Oticon and his Eriksholm eHealth research is partly funded by the Oticon Foundation and the European Horizon2020 programme. Eriksholm has in the last five years received various funds for research from the European Horizon 2020 programme, Volkswagens Stiftung, Oticon Foundation and Wallenberg Foundation. Eriksholm staff are regularly invited as guest speakers at various conferences. Typically they receive travel cost reimbursement, but no speaker fees.




