Open surgery for paediatric airway pathologies such as subglottic stenosis was hailed as revolutionary when many of today’s paediatric ORL specialists were in training. Equipment, facilities and training has moved on and the high-quality optics in modern endoscopes, coupled with greatly refined endolaryngeal instruments and advances in anaesthesia and perioperative care, have brought about a new paradigm shift. Extensive corrective airway surgery without breaching the skin is now a daily occurrence. The team at Great Ormond Street Hospital, London, have been very much to the fore in this area, and two members share some of their experience with us.
The endoscope has long been invaluable in the management of the paediatric airway, both as a diagnostic tool but also to facilitate definitive endoscopic surgery of the airway. In recent years we have seen a resurgence of interest in the endoscope and a shift from purely open reconstructive airway techniques to a combined complementary open and endoscopic approach. Advances in paediatric anaesthesia have allowed for an unhindered view of the airway, and the development of more precise microlaryngeal and endoscopic instruments has increased the scope of endoscopic airway surgery.
Subglottic and tracheal stenosis
Balloon dilation
The management of airway stenosis has evolved considerably, with classic open methods now including open cricoid split and laryngotracheal reconstruction (LTR). Traditional endoscopic methods of dilatation using a bougie with dilators or endotracheal tubes have largely been replaced with endoscopic balloon dilation. Balloon dilation is largely straightforward, is associated with a short procedure time and can be particularly effective for soft immature stenosis of the airway [1] (see Figure 1). The balloon diameter is chosen based on the outer diameter of the ideal sized endotracheal tube for the patients age plus an additional 1-2mm depending on the site of stenosis [2]. Balloon dilation alone can be an effective treatment modality for subglottic stenosis, downgrading the airway stenosis enough to allow for growth of the child, or stabilising the airway prior to open definitive surgery in the form of an LTR or cricotracheal resection (CTR). Additionally, it has a very useful role in the postoperative period following open LTR to prevent early restenosis at graft sites and to keep the airway open.
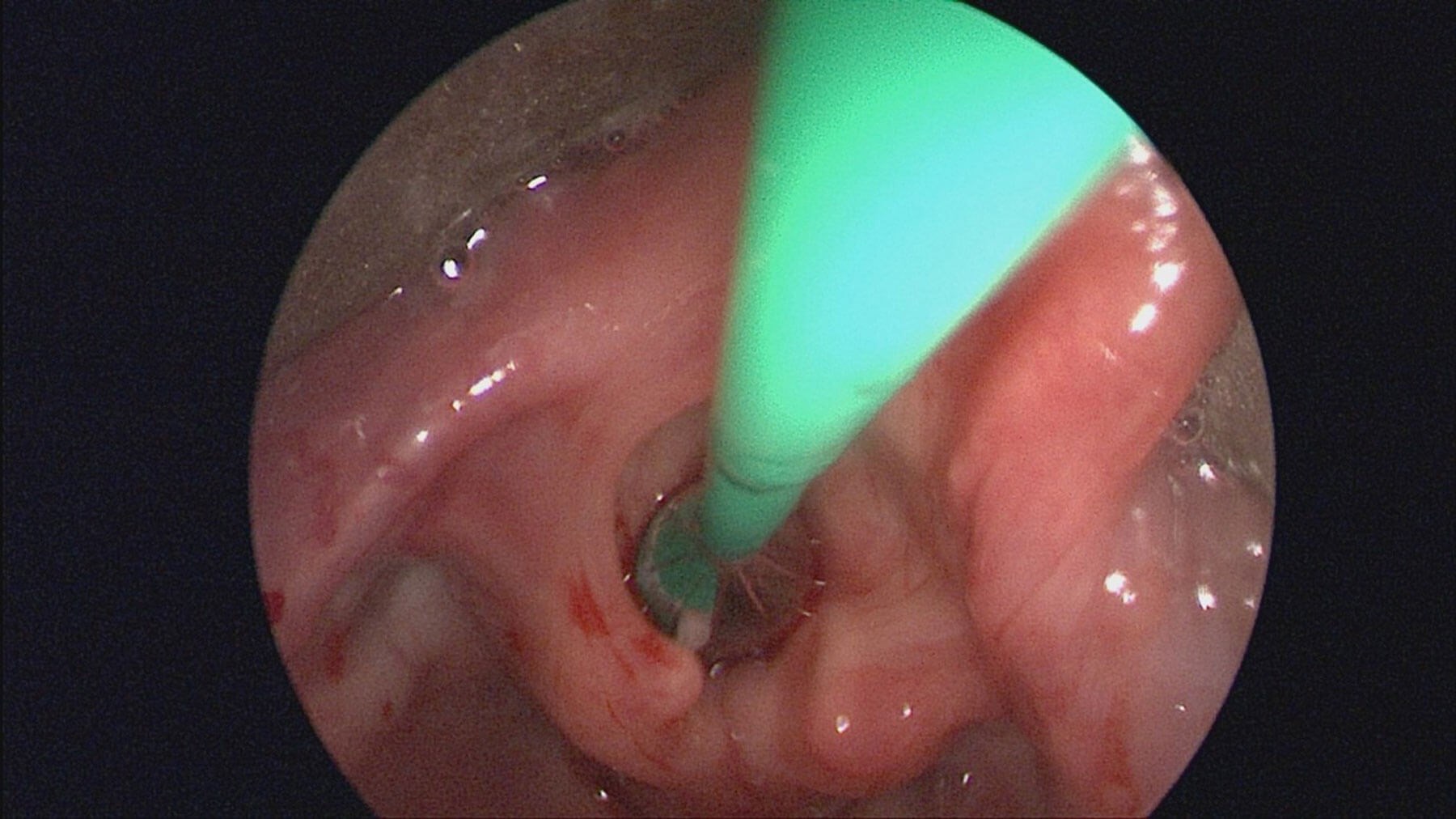
Figure 1. Endoscopic view of larynx with balloon catheter in situ.
Endoscopic cricoid split
Endoscopic cricoid split can be used in selected cases to avoid tracheostomy in neonates who have failed to extubate due to subglottic stenosis. This approach involves intra-luminal division of the cricoid ring using a sickle knife, allowing for expansion of the subglottis and decompression of the airway. The child can then be reintubated for a further period on the neonatal intensive care unit (NICU) with the endotracheal tube acting as a stent.
"The management of airway stenosis has evolved considerably, with classic open methods now including open cricoid split and laryngotracheal reconstruction"
Vocal fold immobility
Bilateral vocal fold immobility, although rare, is the second most common cause of stridor in infants. Anterior and posterior endoscopic split techniques have been shown to be effective in the management of this condition. Whilst the gold standard of management is still tracheostomy, this is not acceptable to a small subset of families and so an alternative approach is sometimes needed. A multi-institutional study of 19 infants treated with endoscopic anterior and posterior cricoid split showed a 73.7% success rate at avoiding tracheostomy or permitting decannulation [3].
Endoscopic posterior graft placement
Reconstruction of the airway with costal cartilage grafts is generally performed via an open LTR technique, however an endoscopic cricoid split can be combined with insertion of a posterior cricoid cartilage graft [4]. This has mainly been effective for children with posterior glottic stenosis, cricoarytenoid joint fixation or bilateral vocal cord paralysis where extra space posteriorly may be enough to avoid tracheostomy or allow for decannulation. Other endoscopic techniques including laser partial arytenoidectomy, cordotomy, and endoscopic suture lateralisation to lateralise the vocal process have also been used in several paediatric centres with promising results.
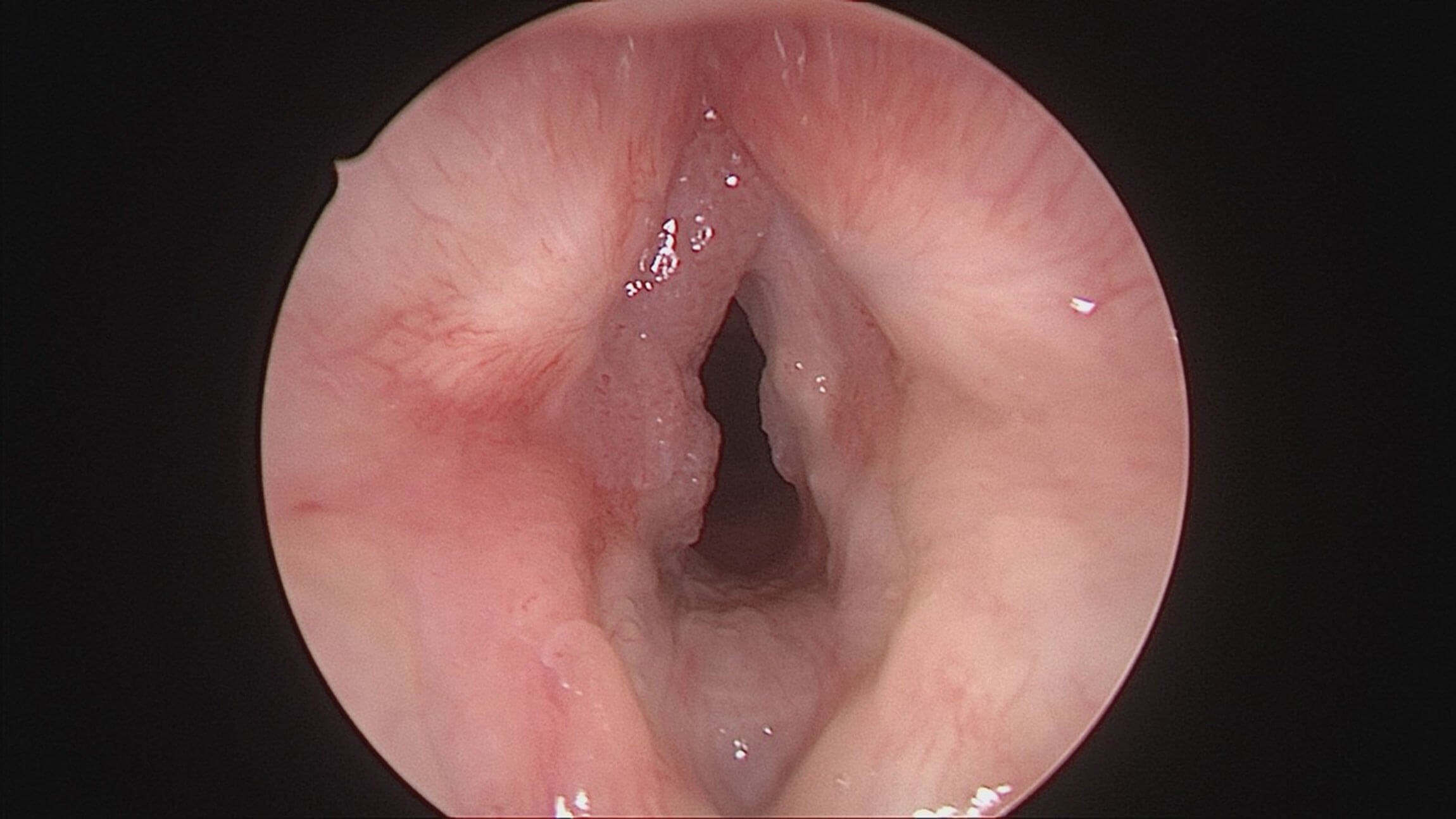
Figure 2. Endoscopic view of larynx showing recurrent respiratory papillomatosis.
Microdebrider
The microdebrider has had a number of applications in ENT and is now commonly used in the sinus and larynx. The laryngeal microdebrider with a skimmer blade is rapidly becoming the modality of choice for recurrent respiratory papillomatosis (RRP). As opposed to the CO2 laser, it is associated with less damage to the normal surrounding tissue, leading to less scarring. Endoscopic visualisation allows for accurate targeting of diseased tissue.
"A multi-institutional study of 19 infants treated with endoscopic anterior and posterior cricoid split showed a 73.7% success rate at avoiding tracheostomy or permitting decannulation"
CO2 laser
The CO2 laser has been a popular option for the management of various airway pathologies, traditionally for RRP. Advances over the years have included more focused and precise delivery of the laser, with handheld aiming devices becoming more popular than the traditional fixed beam on the microscope.The CO2 laser can also be used for the management of suprastomal granulation or collapse, partial arytenoidectomy, cordotomy, scar division, and ablation of tumours within the airway [5].
Adjunctive treatments
Intralesional adjunctive therapies for RRP such as Cidofovir and Avastin can also be administered endoscopically to residual diseased tissue. Application directly to the area or injected directly to the tissue via a spinal needle loaded on a syringe are the methods of choice.
Glottic webs
Glottic webs can be congenital or acquired. Congenital webs may be thick or thin, with the thicker webs also involving a degree of subglottic stenosis. As an important side note, the presence of a congenital web should always raise the suspicion of 22q deletion syndrome; check for other pathognomonic features and/or arrange genetic testing. Acquired webs may be iatrogenic following surgery for RRP, or result from trauma.
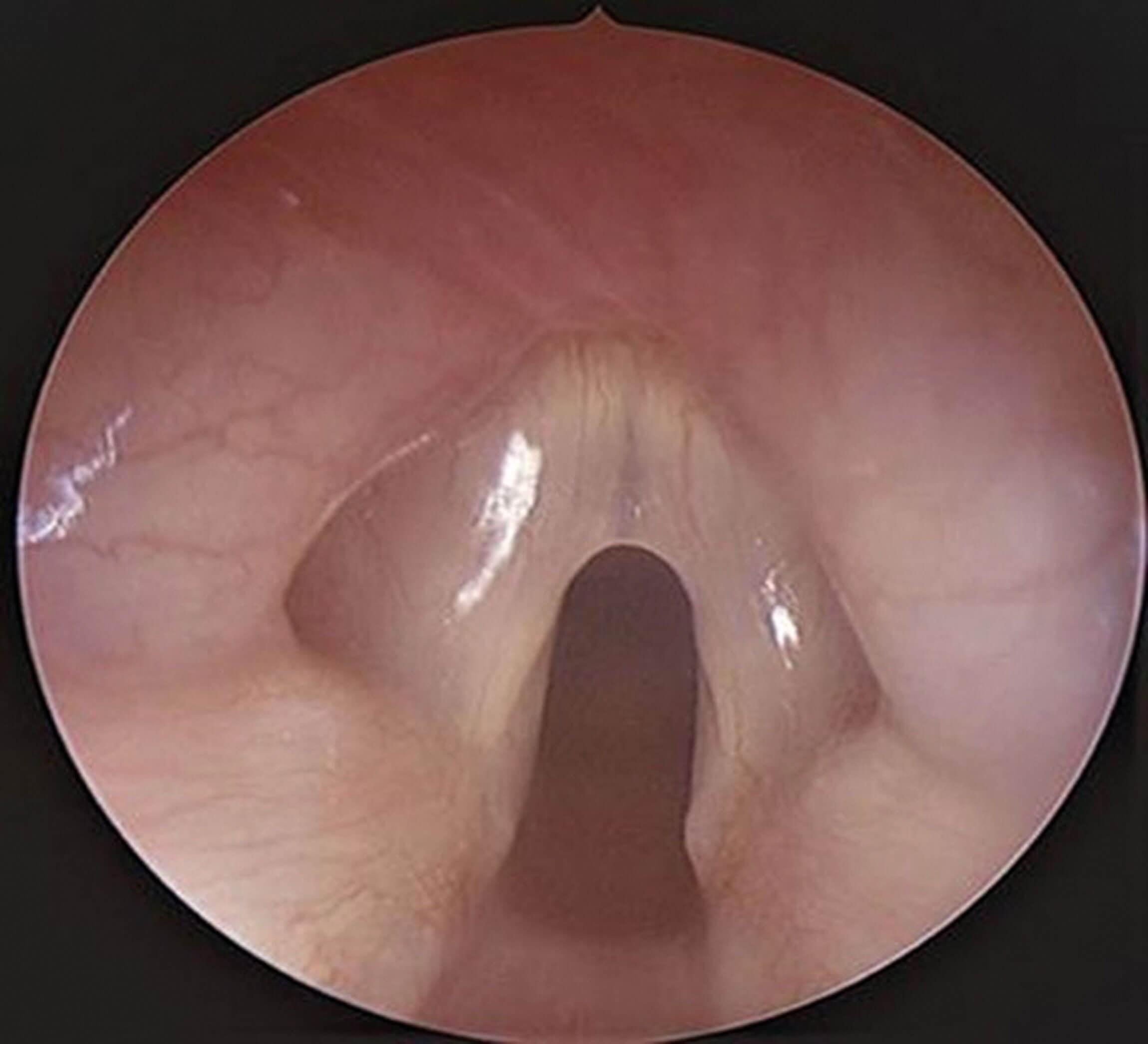
Figure 3. Endoscopic view of larynx showing a thin anterior glottic web.
Division of the web endoscopically (whether as a definitive treatment in itself or combined with open division and expansion of the subglottis) can be particularly accurate, allowing for precise division and visualisation of the vocal cord structures and anterior commissure. Thin webs (Figure 3) may be treated exclusively endoscopically with division of the web, balloon dilation and possible application of pharmacologic agents (Kenolog or Mitomycin C have been reported in the literature). Thicker webs usually require the insertion of a silastic ‘keel’ to act as a stent and this may also be inserted endoscopically or via a combined open and endoscopic procedure. Thicker webs associated with subglottic stenosis or an abnormal cricoid require open surgery with a thyroid alar cartilage or costal cartilage anterior graft.
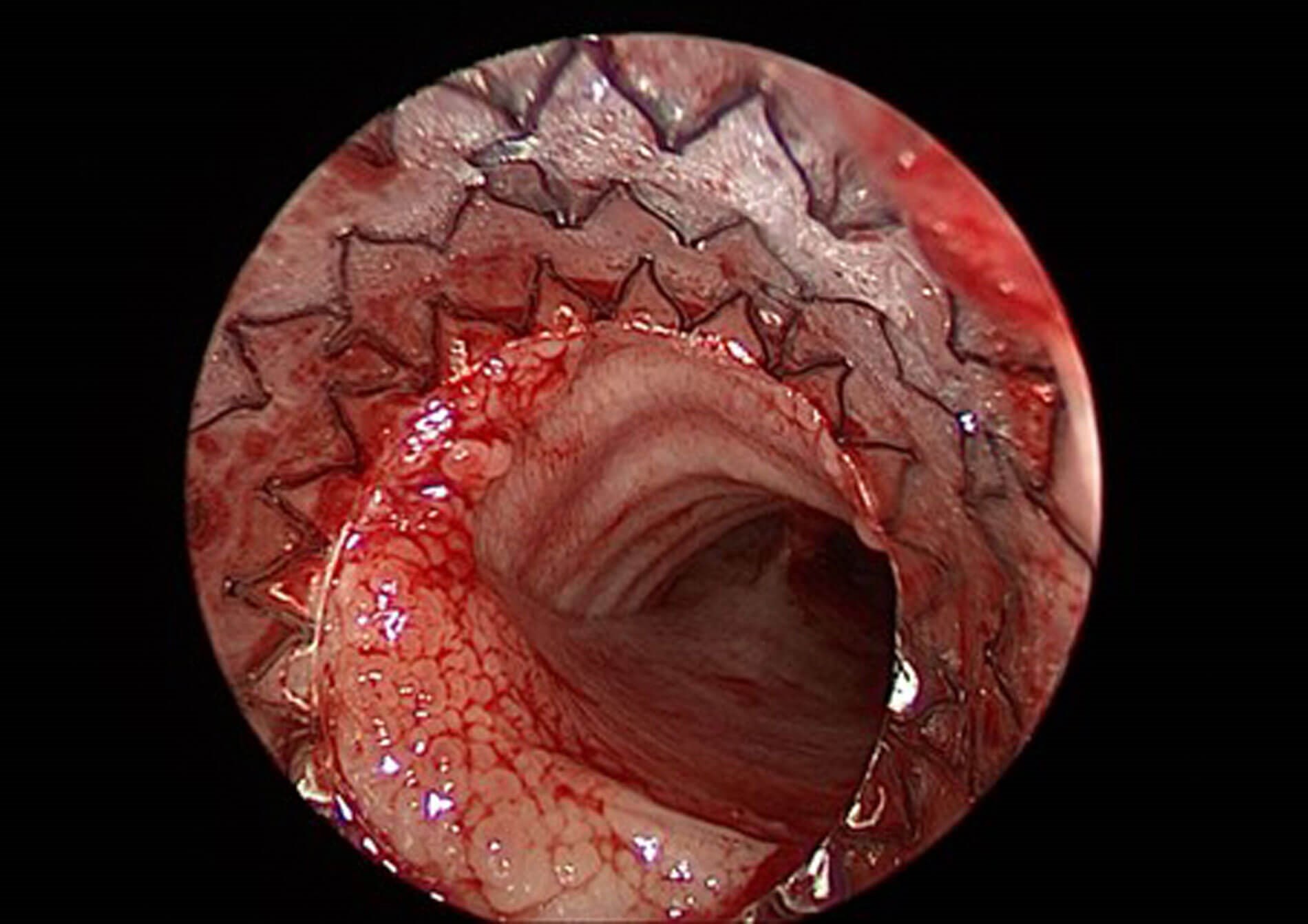
Figure 4. Endoscopic view of airway following AERO-stent deployment for severe malacia.
Tracheobronchomalacia
Intratracheal stents have been used to treat severe malacia, stenosis or compression of the airway when all other options have been exhausted. They are associated with a significant number of complications including granulation formation, migration, and perforation, and should only be used as a temporary measure. Traditional stents have included metal, soft silicone, and biodegradable self-expanding devices. The AERO-stent by Merit Medical is a completely covered self-expanding nitinol stent which has proved an attractive option for these difficult cases (Figure 4). The stent is deployed endoscopically using a pre-loaded delivery system; radio-opaque tip allows for accurate and precise checking of placement.
Laryngeal cleft
Type I, type II, and some short type III clefts can be repaired endoscopically using either a one- or two-layer closure with good success. Removal of a cuff of mucosa from the cleft is essential and can be undertaken using either cold steel techniques or CO2 laser. There is general agreement that outcomes for voice are better following endoscopic repair as this avoids the need for a full laryngofissure with possible disruption of the anterior commissure, which can occur with an open approach.
"Other endoscopic techniques including laser partial arytenoidectomy, cordotomy, and endoscopic suture lateralisation to lateralise the vocal process have also been used in several paediatric centres with promising results"
A deep interarytenoid groove may also require treatment if the child is symptomatic and shows evidence of aspiration. Interarytenoid injection augmentation of a deep groove or a type I laryngeal cleft using sodium carboxymethylcellulose aqueous gel (Radiesse) is a simple management option which is proving popular both as a treatment option and to aid diagnosis. In the United States, injection laryngoplasty is now routinely performed at the time of diagnostic MLB.
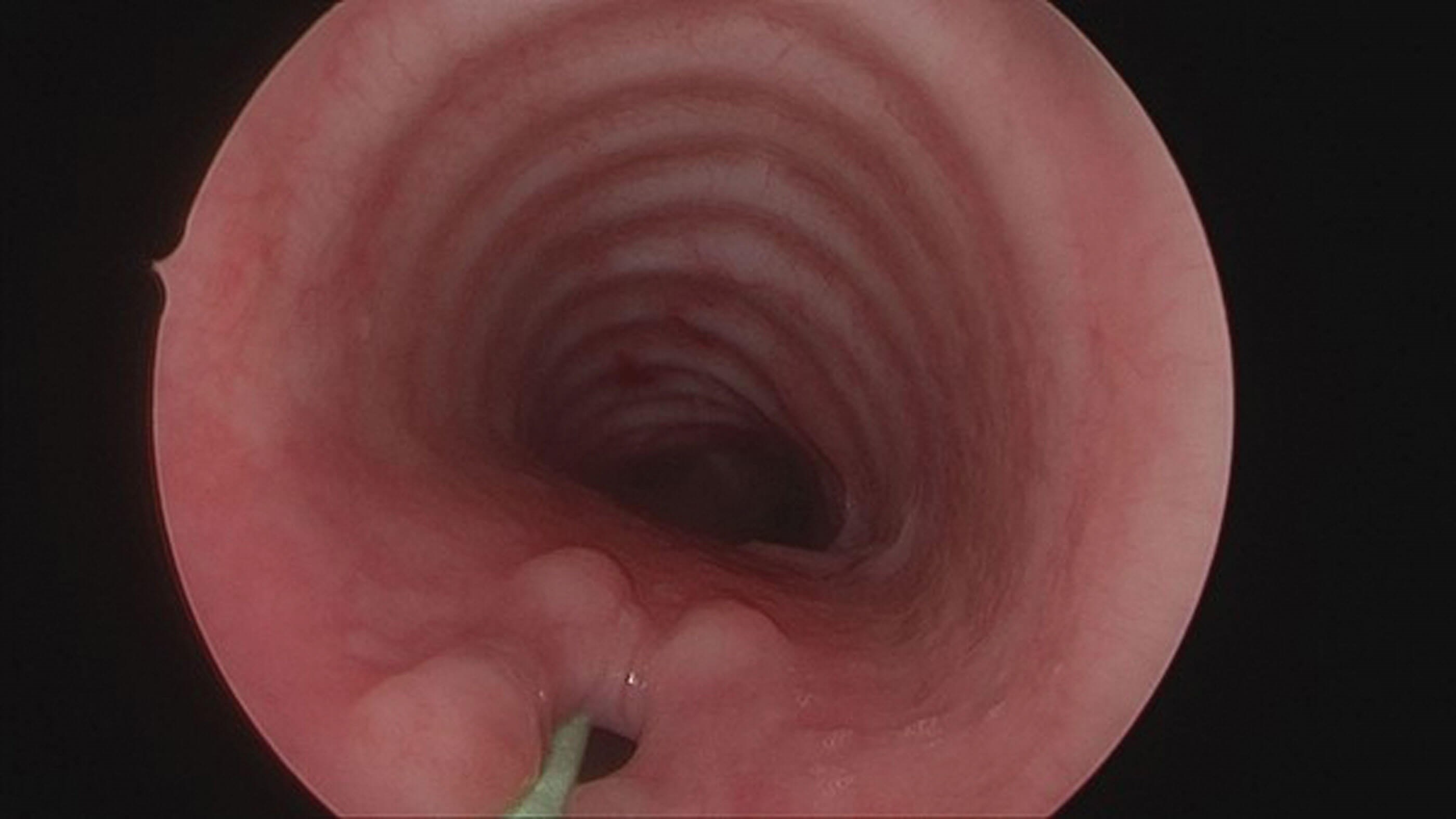
Figure 5. Recurrent tracheo-oesophageal fistula.
Recurrent fistula repair can be managed via an endoscopic approach and broadly involves de-epithelialisation of the tract. This can be carried out using a variety of techniques including diathermy, or cold steel with application of a tissue sealant such as fibrin glue. More recently, the application of trichloroacetic acid to the pouch has proved popular with excellent results. After ‘roughing up’ the mucosa of the tract using a brush or patty, trichloroacetic acid is applied to a small neuro-patty and applied directly to the pouch for roughly 30 seconds. Care is taken to ensure the acid does not come into contact with mucosa within the trachea. Between one to three treatments, approximately four to six weeks apart, are usually required to achieve adequate closure of the pouch.
Conclusion
Endoscopic airway surgery is a key skill for today’s paediatric ENT surgeon. Improved visualisation, instruments and anaesthetic advances mean that endoscopic techniques are now an excellent alternative to open surgery or can be used in a complementary fashion to enhance outcomes in a combined open and endoscopic approach. With further technological advances on the horizon, the future of endoscopic airway surgery is bright.
References
1. Avelino M, Maunsell R, Jube Wastowski I. Predicting outcomes of balloon laryngoplasty in children with subglottic stenosis. Int J Pediatr Otorhinolaryngol 2015;79(4):532-6.
2. Jefferson ND, Cohen AP, Rutter MJ. Subglottic stenosis. Semin Pediatr Surg 2016;25(3):138-43.
3. Rutter MJ, Hart CK, Alarcon A, et al. Endoscopic anterior-posterior cricoid split for pediatric bilateral vocal fold paralysis. Laryngoscope 2018;128(1):257-63.
4. Inglis AF Jr, Perkins JA, Manning SC, Mouzakes J. Endoscopic posterior cricoid split and rib grafting in 10 children. Laryngoscope 2003;113(11):2004-9.
5. Lee GS, Irace A, Rahbar R. The efficacy and safety of the flexible fiber CO2 laser delivery system in the endoscopic management of pediatric airway problems: Our long term experience. Int J Pediatr Otorhinolaryngol 2017;97:218-22.












