Necrotising otitis externa is increasing in incidence in the UK and becoming a rising burden to patients and health services. Despite a growing body of literature on this condition, we know very little about patient experience of necrotising otitis externa. Eloise Owen set out to remedy this gap in our knowledge, with her qualitative study on the theme.
Necrotising otitis externa (NOE) is an aggressive infection of the external auditory canal, which can spread to the skull base. Typically, it affects immunocompromised, diabetic, and elderly patients. It can have destructive consequences, including facial nerve palsy, compromised hearing, and meningitis.
Although NOE is typically uncommon on a day-to-day basis, it is important to be aware of this disease, not only because the number of cases are on the rise [1], but due to the debilitating effect on patients. A qualitative study conducted at Manchester Royal Infirmary, UK, has discovered the patient perspectives of NOE, and is the first study to do so [2]. This article will explain the results of this study, revealing the true impact that NOE has on patients’ lives and demonstrating the need for a patient-centred approach when dealing with the infection.

Figure 1. Quotes from NOE patients.
Extreme, relentless pain is a key feature that clinicians should be aware of when treating NOE. Almost all patients will have head pain, and usually pain in other locations including the jaw, ear, face, and neck. Patients have reported that the jaw pain causes difficulties in eating. This is concerning given that the patients are already frail, and usually diabetic. The pain is worse at night time and, because of this, it leads to fatigue. It is imperative that patients receive sufficient analgesia in proportion to their pain. Patients often state that over-the-counter pain relief is unsatisfactory, resulting in feelings of desperation, causing the potential risk of overdose.
“Patients often state that over-the-counter pain relief is unsatisfactory, resulting in feelings of desperation, causing the potential risk of overdose”
NOE can leave extreme impressions on patients’ mental health. Patients can experience depression and low mood, suicidal thoughts, and feel anxious about relapse of symptoms. Figure 1 shows four patient quotes from NOE patients. The grave impact that NOE has on patients’ mental health is concerning, and holistic care of the patient must not be missed. Patients’ moods can get so low, and this can lead to suicidal ideations.
Patients have a poor quality of life whilst suffering with NOE. Both pain and decline in mental health contribute to a deterioration in quality of life for the patient, but there are also other responsible factors which are shown in Figure 2. NOE is debilitating for patients; it causes hearing difficulties, weight loss (due to the pain caused by eating, they are unable to eat), ear discharge, dizziness, hearing difficulties and disrupted sleep. We must be aware that NOE is more than just an ear infection, and we should appreciate the entire impact it has on the patient. Furthermore, NOE can disrupt relationships with family and friends.
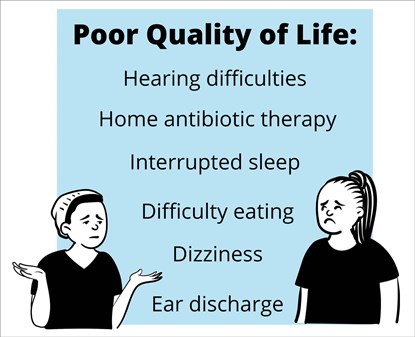
Figure 2. Factors responsible for poor quality of life in NOE patients.
Patients say they do not want to interact with their family, due to the pain, fatigue, and low mood, and that they also feel like a burden, due to the heightened amount of care they now require. The treatment for NOE is typically IV antibiotics for six to eight weeks [3]. These antibiotics are usually started in hospital then, once the patient is discharged, continued at home. Patients have stated that though it is a large inconvenience having a nurse coming to the house for treatment every day, they are grateful that this care can be received at home rather than in hospital.
“It is important to be aware of this disease, not only because the number of cases are on the rise, but due to the debilitating effect on patients”
Delays in receiving a diagnosis of NOE is something that many patients experience. Whether this be in the primary care setting or the hospital, it leaves patients feeling frustrated and defeated. Patients said they visited their community doctor numerous times before getting referred to the hospital. During this time, they are experiencing a lot of pain. The longer NOE remains untreated, the bigger the risk of damaging consequences (cranial nerve damage, meningitis, intracranial abscess), and the greater the negative impact on their quality of life and mental health. It is therefore important that primary care clinicians are aware of NOE, especially when they see a diabetic or immunocompromised patient with otitis externa that is unresponsive to initial treatment, or if the patient is in a disproportionate amount of pain. In the hospital environment, it is crucial for prompt diagnosis (doing scans and taking cultures when needed) so that patients can be started on treatment quickly and given sufficient analgesia.
To conclude, patients with NOE will have a considerable pain, a decline in quality of life and mental health, and they will experience long diagnostic delays. It is crucial that NOE is recognised early and treated promptly. This will improve the patient experience and lead to better patient outcomes.
References
1. Chawdhary G, Liow N, Democratis J, Whiteside O. Necrotising (malignant) otitis externa in the UK: a growing problem. Review of five cases and analysis of national Hospital Episode Statistics trends. J Laryngol Otol 2015;129:600-3.
2. Owen E, Abrar R, Stapleton E. Patient Experience of Necrotising Otitis Externa: a Qualitative Study. [Manuscript submitted for publication] 2021.
3. Chawdhary G, Pankhania M, Douglas S, Bottrill I. Current management of necrotising otitis externa in the UK: survey of 221 UK otolaryngologists. Acta Otolaryngol (Stockh) 2017;137:818-22.