Whilst vestibular dysfunction is a known outcome of cochlear implant surgery, do we know the risk factors associated with this, particularly in children? In this article a team from University of Tokyo discuss their findings.
Cochlear implantation (CI) is an effective treatment for severe-to-profound sensorineural hearing loss (SNHL). Bilateral CI has been reported to be beneficial for sound localisation and preverbal communication and language development, particularly in paediatric cases, which results in an increasing number of SNHL patients with bilateral CI. However, CI can be harmful to inner ear function such as vestibular function, and there is a growing concern about vestibular impairment after CI, especially in bilateral CI children.
Considerable efforts have been devoted to relieving this vestibular damage after CI, both by otologists and by manufacturers. Surgical approach improvement and CI electrode upgrading have been two major approaches for this purpose. Several mechanisms have been suggested for vestibular dysfunction due to CI, including traumatic injury, fibrosis, electrical stimulation of the otolithic organs, perilymph fluid leakage, and labyrinthitis due to foreign body reaction [1]. Histopathological studies have shown that CI insertion affects vestibular function by inducing fibrosis in the vestibule, saccule membrane distortion, and cochlear and vestibular hydrops. Classically, a CI electrode has been inserted into the hole which was drilled on the outer wall of the cochlear. This approach - cochleostomy - could cause fibro-osseous reaction and scala vestibuli fibrosis, resulting in vestibular endolymphatic hydrops [2]. On the other hand, recently the CI electrode is inserted through a round window (RW) membrane. When the RW membrane is difficult to be seen, the surrounding bone is drilled out to expose the RW membrane and make it easy to insert. These approaches, RW approach or extended RW approach, are reported as less damaging to the inner ear structures.
An electrode type also plays a vital role in avoiding inner ear trauma. A perimodiolar electrode has been used to make the electrode close to the spiral ganglion cells which were targets of electrode stimulation but, after a thin straight type of electrode was developed, a temporal bone study suggested that the use of a straight electrode minimised trauma to the intracochlear structures and was less traumatic to the inner ear. A straight electrode has a less likely incidence of translocation from the scala tympani to the scala vestibuli, all of which cause damage to the osseous spiral lamina or basilar membrane in the cochlear basal turn and are highly correlated with vestibular damage [3].
Various reports have demonstrated the superiority of RW approach [4] and the straight electrode [5] in cochlear preservation by estimating residual hearing ability. As to vestibular function, several studies or meta-analysis showed that RW approach and the straight electrode was related to a lower incidence of vestibular dysfunction after CI. However, most of the data in the studies included in their meta-analysis were obtained from adult patients, so the identity of the risk factors for vestibular impairment in children remains unclear. Therefore, we estimated the deterioration of vestibular function after CI in paediatric patients and identified the risk factors for vestibular dysfunction.
We routinely perform caloric testing, cervical vestibular-evoked myogenic potential (cVEMP) testing, and damped rotation testing to evaluate vestibular function before CI, even in children. In patients undergoing sequential bilateral CI, identical vestibular tests are performed for both ears. Using these data, we could compare the vestibular function of the first implanted ear before and after the procedure.
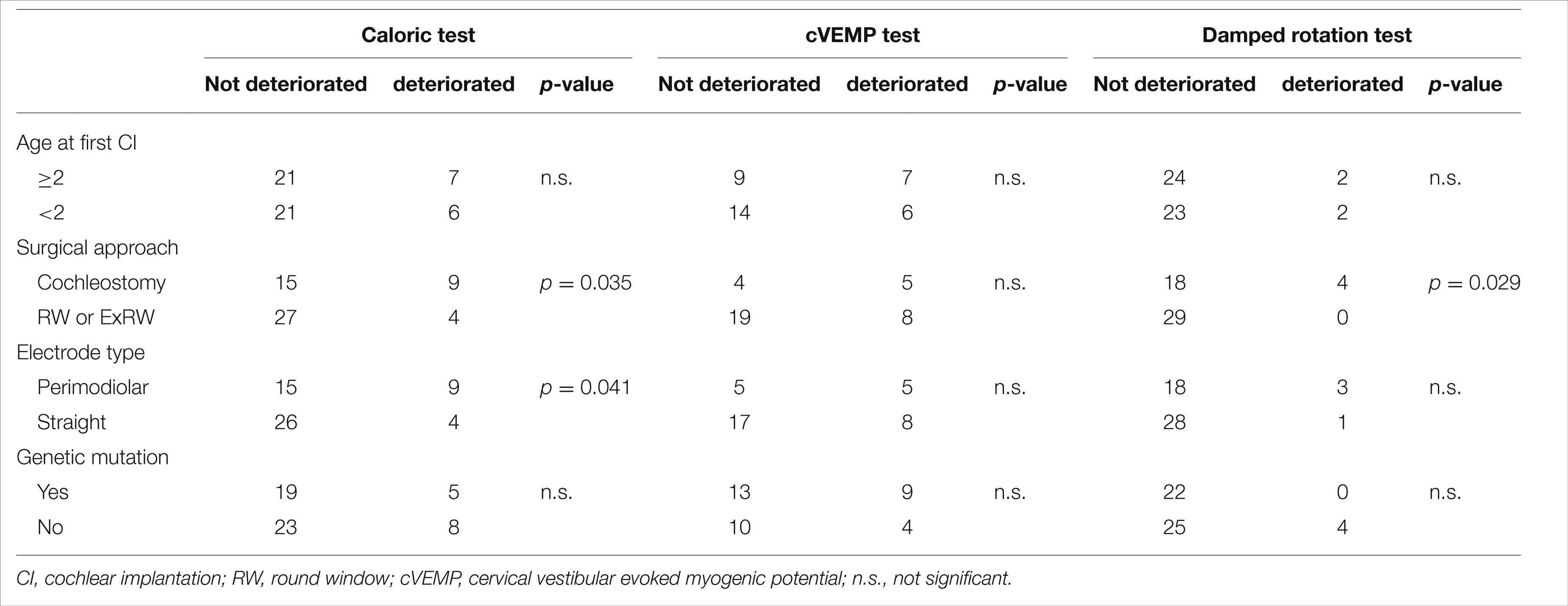
A total of 73 children (male: 38, female: 35, mean age: five years and seven months ± three years and six months) who underwent sequential CI were included in this study. The mean age at preoperative evaluation was two years and eight months (range: five months to 12 years). We classified the response in each vestibular function test, caloric test, cVEMP test, and damped rotation test, as positive, weak, or negative. Vestibular function deterioration was defined when the patients had a positive or weak response before surgery that dropped to a weak response or no response after surgery in each vestibular test. We used Fisher’s exact test to assess the risk of each independent variable and the differences among each vestibular test. Statistical significance was set to p < 0.05.
Deterioration of test results was most frequently observed in the cVEMP test (36.1%), followed by the caloric test (23.6%), and then the damped rotation test (7.8%). The deterioration of vestibular function based on each test was compared with age at implantation, surgical approach, electrode type inserted, and the existence of genetic mutations (See Table). Age and the existence of genetic mutations did not affect any of the vestibular test results. On the contrary, cochleostomy significantly deteriorated caloric test and damped rotation test reaction, and perimodiolar electrode significantly decreased caloric test reaction.
Our finding that a straight electrode with an RW or extended RW approach would be preferable to preserve vestibular function is the same as the result among adults, but children with SNHL tend to receive bilateral CI due to bilateral hearing benefit, and the need for preservation of vestibular function is increasing. Therefore, an RW or an extended RW approach with straight electrodes is desirable to preserve vestibular function after CI, especially for children [6].
References
1. Licameli G, Zhou G, Kenna MA. Disturbance of vestibular function attributable to cochlear implantation in children. Laryngoscope 2009;119(4):740-5.
2. Ishiyama A, Doherty J, Ishiyama G, et al. Post hybrid cochlear implant hearing loss and endolymphatic hydrops. Otol Neurotol 2016;37(10):1516-21.
3. Tien HC, Linthicum FH. Histopathologic changes in the vestibule after cochlear implantation. Otolaryngol Head Neck Surg 2002;127(4):260-4.
4. Hansel T, Gauger U, Bernhard N, et al. Meta-analysis of subjective complaints of vertigo and vestibular tests after cochlear implantation. Laryngoscope 2018;128(9):2110-23.
5. Dhanasingh A, Jolly C. An overview of cochlear implant electrode array designs. Hear Res 2017;356:93-103.
6. Koyama H, Kashio A, Fujimoto C, et al. Alteration of Vestibular Function in Pediatric Cochlear Implant Recipients. Front Neurol 2021;12:661302.