We as doctors do not always know the answer. Associate Professor Jacqueline Allen guides us through the importance of acceptance of this uncertainty and its complex mental journey. She highlights that, as clinicians, we must embrace the unknown and be honest to the patients whom we serve.
We spend years training at medical school, then as a junior doctor and then in a training programme to become a specialist, often followed by a fellowship. For most, this journey takes the better part of 15 years and the prospect of being the ‘final decision maker’ is still a daunting one! Patients have expectations of us: ‘Doctors are knowledgeable’; ‘Specialists are confident and make the correct decision - they know what they are doing’.
We want to be sure ourselves, we don’t want to admit uncertainty – this might tarnish our glow, the belief that patients have in us. It takes a lot of guts to admit that you, as the specialist, are uncertain or do not know the best course of action. Sometimes this is because there is no one best course of action – in other words, it cannot be easily determined which course will provide the best outcome. A more frightening alternative is when no obvious course of action presents itself to you and you are left wondering just what, if anything, you can offer. A feeling of being empty-handed in the face of a patient expecting and hoping to ‘see the best specialist in the field’ is demoralising and, for many of us, anxiety-provoking. John Huston Finley said, “maturity is the capacity to endure uncertainty” and, in the context of medical care, you need to be self-assured enough and humble enough to not view ‘not knowing’ as a failing or a weakness. It is crucial to practise self-examination and maintain a strong connection to other colleagues who can keep you grounded and help to avoid isolation.

Transnasal endoscopic view of gastroesophageal junction
demonstrating hiatus hernia and Shatzki’s ring.
Uncertainty, whilst disconcerting, can provide the impetus to develop new ideas, new skills and to innovate. As Ilya Prigogine said, “the future is uncertain…but this uncertainty is at the very heart of human creativity”. If we see an opportunity, rather than a problem, we can take uncertainty into our hearts and use it to drive and implement change and growth. This is the reason why most medical systems support senior doctors taking sabbaticals; so that they still have the chance to expand their knowledge, be inspired to continue working in a creative way and to appreciate newly developing therapies. We need to remember that the “opposite of certainty is not uncertainty. It’s openness, curiosity and a willingness to embrace paradox…” - Tony Schwartz.
In laryngology, where I spend my days, while we know many things (the larynx forms from the foregut, the glottis is a valve, airway protection comes ahead of phonatory function), there are many areas of uncertainty. Why does one heavy smoker develop Reinke’s oedema of the vocal fold and another smoker, a glottic cancer, and the Reinke’s never becomes carcinoma? Why does spasmodic dysphonia develop? How much acid is too much acid – in the stomach? In the lower oesophagus? In the pharynx? Does pepsin cause laryngeal cancer? How much is enough collagen in the superficial lamina propria? Researchers examine these areas in laboratory work and through studies as best they can but, day to day when we see patients, a clinician needs to navigate these unknowns and deal with uncertainty, making decisions about clinical care appropriate to each individual.
We need to acknowledge and recognise uncertainty. It takes time to work out a process to deal with your own uncertainty and sometimes, think outside the box. By recognising where we lack a strong evidence base, we can be inspired to challenge the status quo or to consider alternative strategies.
"If we see an opportunity, rather than a problem, we can take uncertainty into our hearts and use it to drive and implement change and growth"
We also need to acknowledge and admit to patients when we don’t know. We are then justified in still offering our opinion regarding management, whether we have developed that based on probabilities, combined experience, gut instinct or just choosing from the options that we have at our disposal. Sometimes we can call a friend, refer to another colleague or different centre where additional expertise may be available. At least if we are honest with the patient, they can be party to the decision-making process and give weight to the unknown at their own level of tolerance, decide for themselves whether trying something with a less clear risk-to-benefit ratio is appropriate for them. In this arena also enters the truly novel and experimental options – those that are on trial and explicitly so. The patient should always know that these are not conventional, that this particular treatment option is no more sure than a flip of a coin at best, and that you are offering this based upon there being no other safer option or more reliable strategy for achieving an effective outcome. While uncertainty can bring paradigmatic changes if it inspires innovative thinking, an individual patient cannot and should not have to accept the risks of unexplored therapies when reliable safe options exist, without explicitly choosing to do so.
As clinicians, our responsibility is first to do no harm.
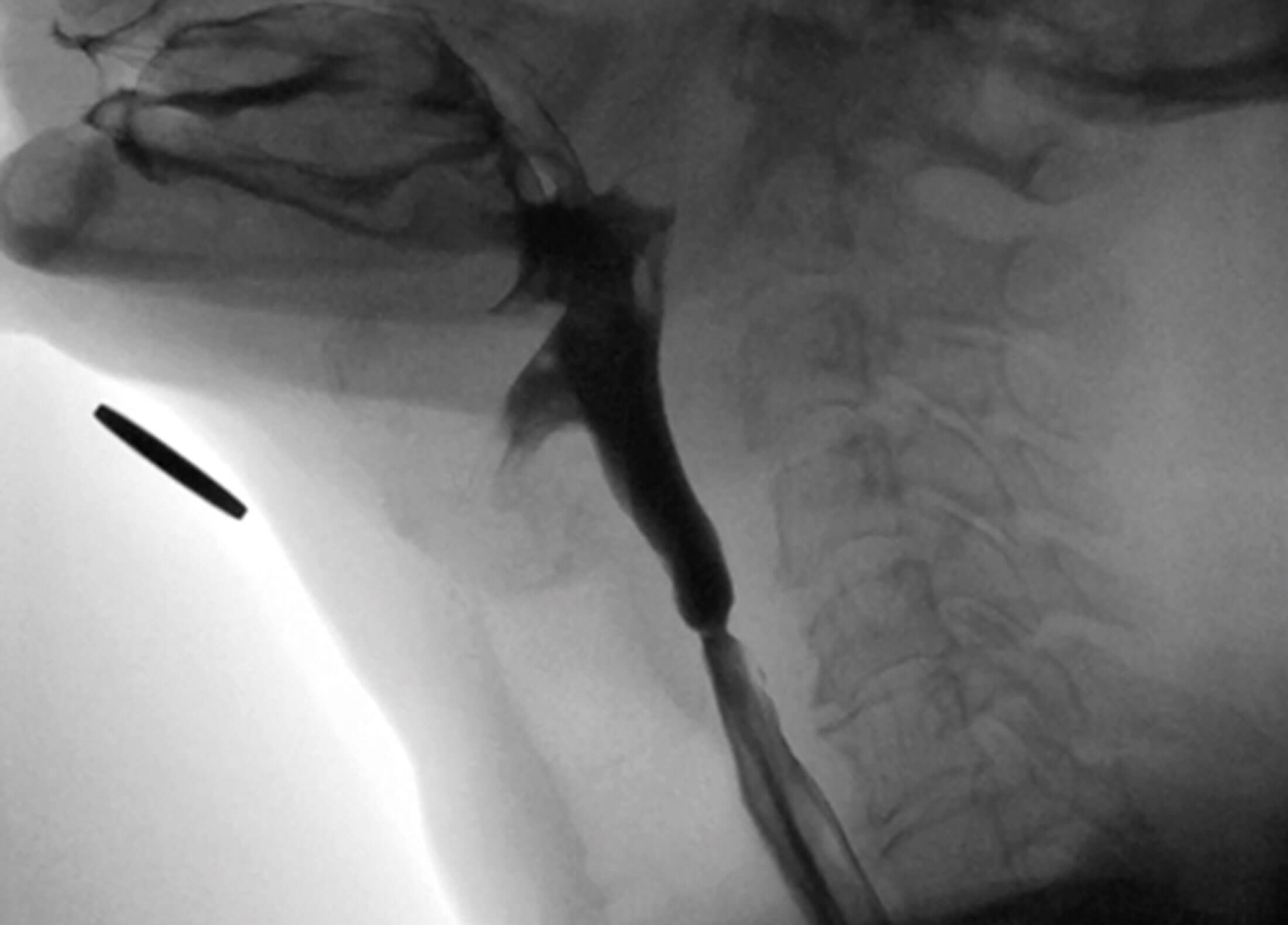
Fluoroscopic lateral view of pharyngoesophageal segmaent
demonstrating upper oesophageal sphincter web.
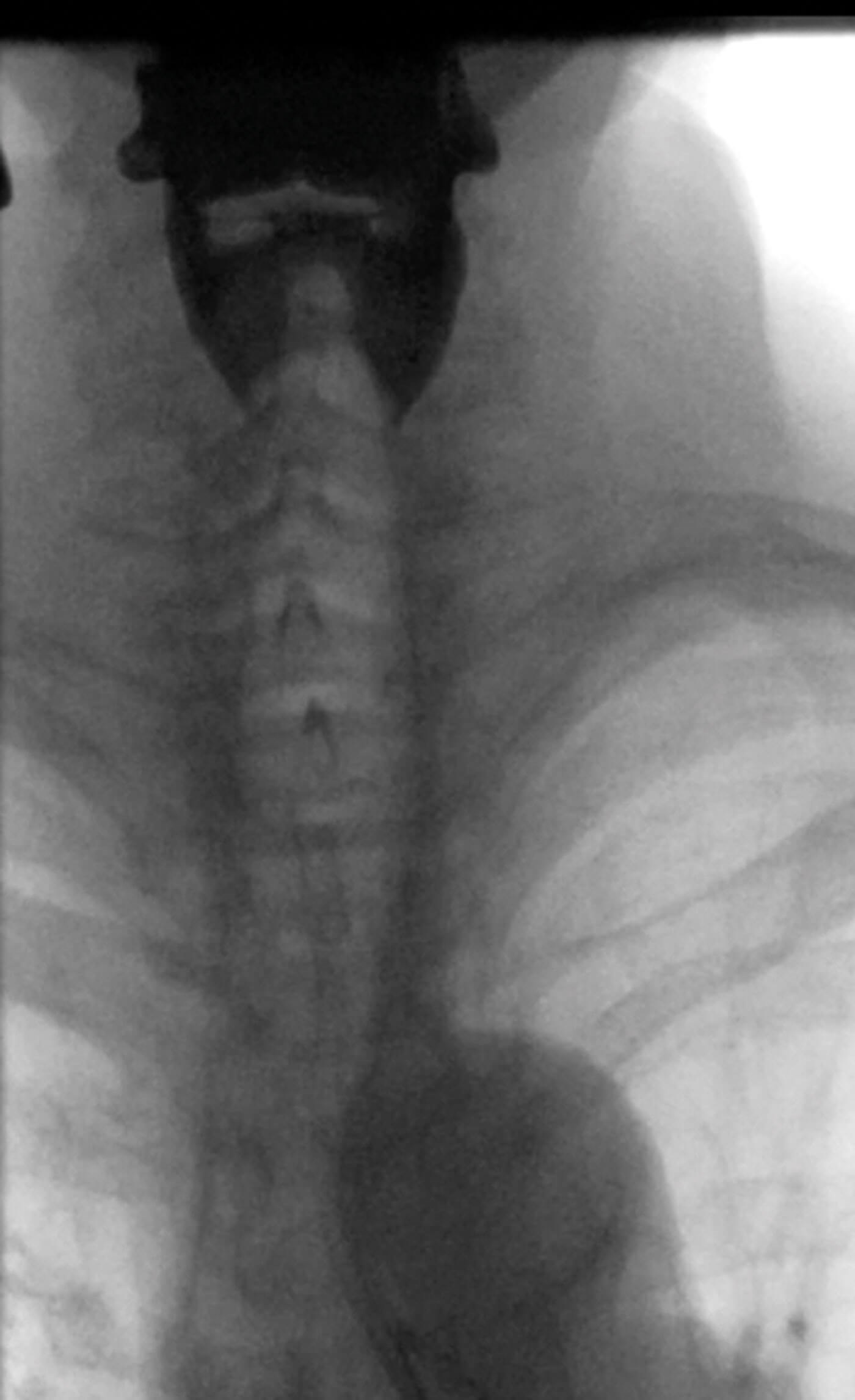
Fluoroscopic image of bilateral high pharyngeal diverticuli (white diverticuli)
that typically drain spontaneously and are asymptomatic.
Clinicians also need to consider outcomes from the patient’s perspective. Of course, it is only the patient that can tell whether the cure is better than the ailment; however, often this is only in retrospect. At the time of treatment choice, the clinician needs to advocate for the outcomes most acceptable to the patient (and therefore, the management strategy that can achieve it). Removing your own personal bias from this decision making can be difficult and, at times, uncertainty impacts this process. When there are seemingly multiple random outcomes possible, we may tend toward conservatism – a defensible position!
Personally, my approach to uncertainty is to remember I don’t know everything, consider the worst-case scenario in my suggested treatment, whilst trying to avoid harm and minimise risk, and then to have an honest discussion with the patient about the ambiguity and reach a consensus together. At least then, there is joint responsibility and buy-in for novel or non-conventional therapies. Never stop questioning why, and be open to new ideas, no matter from whom they come. “Learning is a matter of gathering knowledge; wisdom is applying that knowledge” - Roopleen.