In this article, the authors introduce the description of swallowing problems which have been recently attributed to muscle tension dysphagia (MTDg). The authors are clear that this is a diagnosis of exclusion, and it is important to rule out other causes of dysphagia.
There is a challenging group of patients who report a significant impact on quality of life due to swallowing difficulties, yet comprehensive assessment reveals no underlying aetiology for the swallowing complaint. These patients undergo multiple specialist evaluations with no diagnosis or treatment offered, thus resulting in increased anxiety and even fear of swallowing.
It has been our clinical experience that these patients with ‘idiopathic functional dysphagia’ actually reveal excessive laryngeal muscle tension that is observable during laryngoscopy and during paralaryngeal and circumlaryngeal palpation. Based on this clinical observation, Kang et al. introduced muscle tension dysphagia (MTDg) as a diagnostic taxonomy in 2016, allowing patient-centred diagnosis and care. The most common patient-reported symptoms of MTDg are difficulty swallowing solids, throat discomfort with swallowing, and the sensation of food sticking in the throat, among others. Currently, MTDg is a diagnosis of exclusion after proper instrumental dysphagia screening, ruling out other possible causes, such as oesophageal webbing and malignancies of gastroenterologic nature [1].
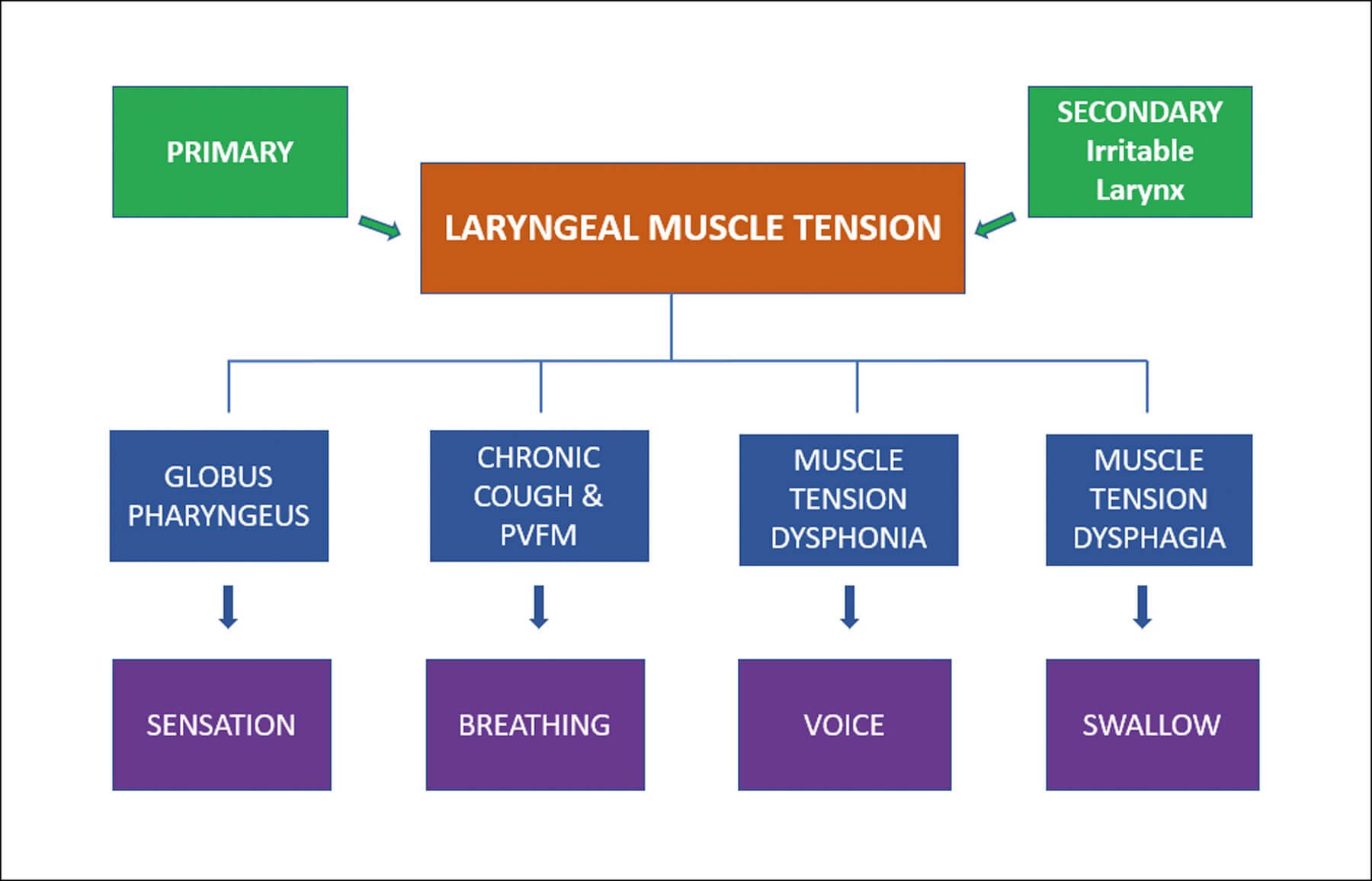
Figure 1. Flowchart demonstrating the spectrum of muscle-tension laryngeal disorders.
Although MTDg can occur with or without concomitant laryngeal disorders, studies conducted by Kang et al. in 2016 and 2021 revealed that many patients with suspected MTDg also exhibited a spectrum of muscle tension-based laryngeal disorders known as ‘irritable larynx syndrome’ (Figure 1). This syndrome is an umbrella of conditions related to the primary functions of the larynx: sensation, breathing, voice and swallow. These disorders may manifest as muscle tension dysphonia, paradoxical vocal fold motion, chronic cough, chronic throat clearing, and globus pharyngeus (‘lump in the throat’) [2]. Recent research has elucidated that excessive laryngeal musculoskeletal activity serves as the underlying factor in muscle tension-based laryngeal disorders. Patients exhibiting only the signs and symptoms of difficulty swallowing were designated the classification of primary MTDg, whereas patients presenting with other concomitant muscle tension-based ‘irritable larynx’ disorders were designated the classification of secondary MTDg [1,3].
MTDg has incorrectly been referred to as a symptom of muscle tension dysphonia (MTD) in some circles since supraglottic muscle tension in dysphonia patients with swallowing complaints has been commonly observed. Despite the strong coincidence between MTD and MTDg shown in our research and that of others [1,3,4], our research has shown that they are mutually exclusive. In other words, these patients do not always complain of dysphagia and dysphonia at the same time, nor do they necessarily exhibit signs of dysphonia in conjunction with the dysphagia complaint [1,3].
In order to best assess patients with excessive laryngeal muscle tension, a practitioner must pay attention to the biomechanics of the larynx, not just the structural abnormalities. Laryngoscopy is a useful tool to assess structural pathology, but it is underutilised in assessment of laryngeal muscular function. Patients often report being told that there are ‘no lumps or bumps’ in their throats and that they are overthinking things, despite demonstrating signs of significant laryngeal muscle tension on laryngoscopy and visual inspection. Clinicians should be familiar with signs of muscle tension, such as supraglottic compression, paradoxical vocal fold motion, and arytenoid quivering (see video at https://bit.ly/3m2Hknm).
Therapy aimed at unloading laryngeal muscle tension results in complete symptom resolution, or significant symptom improvement, in the vast majority of patients. The 2016 study by Kang et al. demonstrated symptom resolution or improvement in 100% of patients who had therapy for laryngeal muscle tension [1]. The 2021 study by the same group showed that an average of four speech-therapy sessions focused on unloading laryngeal muscle tension resulted in 90% symptom resolution for MTDg patients by the completion of therapy. Interestingly, patients with a diagnosis of reflux who did not find symptom relief with appropriate proton pump inhibitor (PPI) therapy, had a mean dysphagia symptom improvement of 96.6%. The study results suggest that the dysphagia symptoms in this group of patients have a high association with laryngeal muscle tension and that reflux alone is not the cause in most patients [3].
For some clinicians, it may be difficult to find a speech-language pathologist versed in treatment of laryngeal muscle tension disorders. Although not documented by research, some providers report to the authors their ability to assist patients by referring them to physical therapy, myofascial release therapy, anxiety management, and stress-reduction counselling. It is important to note that swallow strengthening exercises are absolutely discouraged per our clinical experience as can they make the laryngeal muscle tension worse.
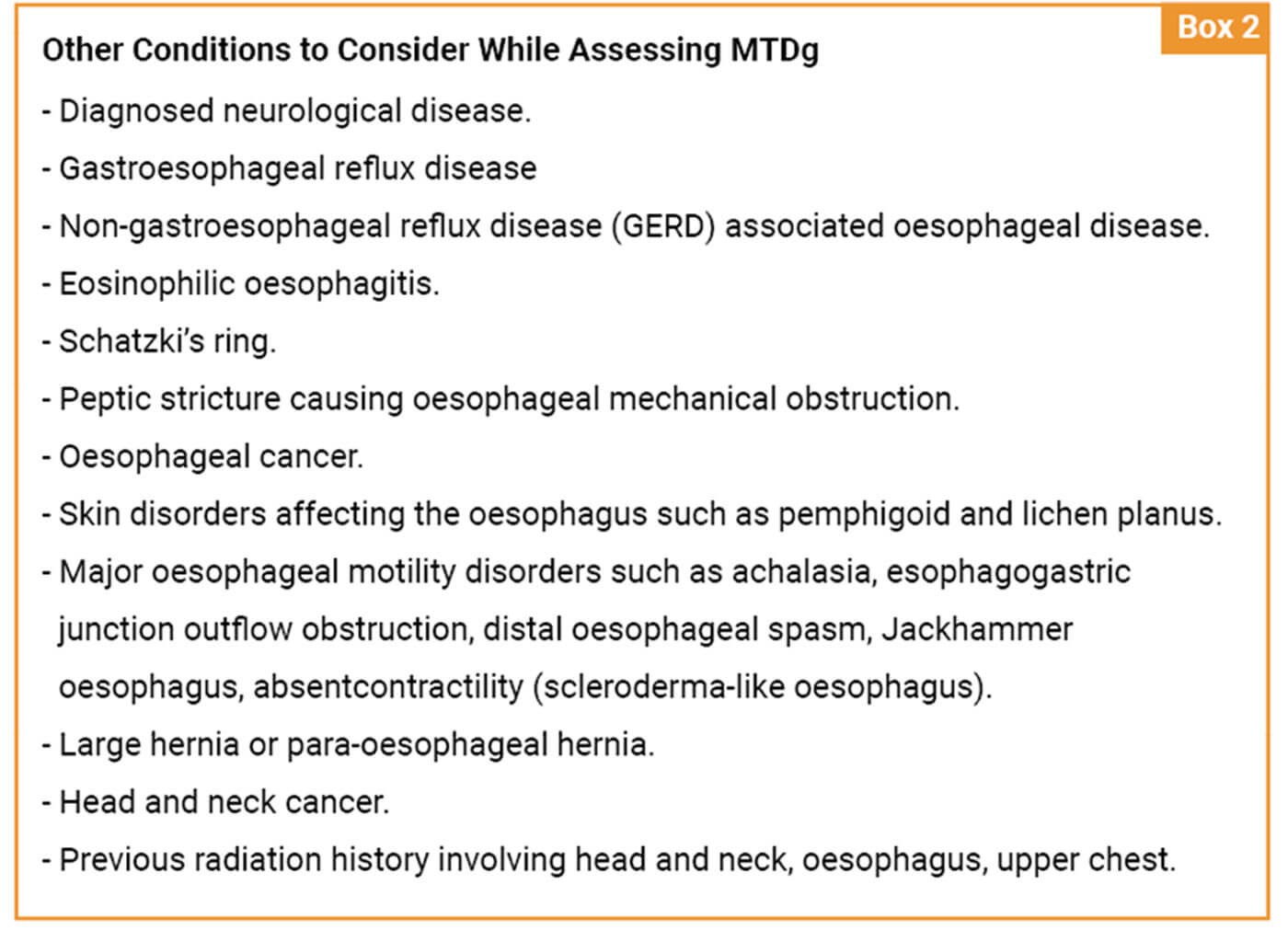
Since the introduction of MTDg as a clinical entity, there has been controversy regarding how much testing is necessary and appropriate for efficient and cost-effective diagnosis and treatment. There is understandable concern that patients might receive a diagnosis of MTDg without proper workup, resulting in a missed diagnosis of structural pathology, such as an oesophageal cancer. However, MTDg is a diagnosis of exclusion only arrived at after patients have undergone many objective laryngeal and gastroenterological tests (Box 1).
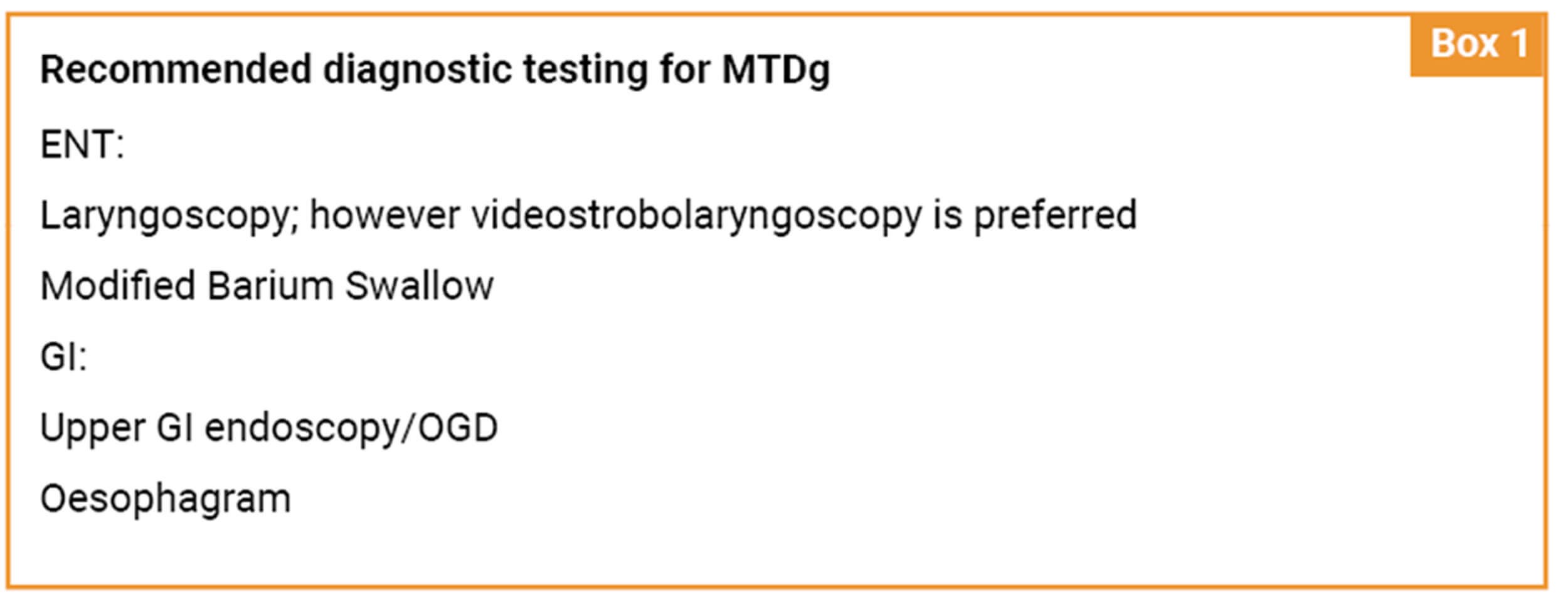
As such, it can be a costly and time-consuming diagnosis. The question of efficacy and the need for multiple tests also arises for younger patients who are not normally considered at risk for gastroenterologic malignancies. Ultimately, it is the providing clinician’s judgment to determine which patient population requires specific testing based on their risk factors and presenting symptoms (Box 2).
Undergoing four sessions of laryngeal rehabilitation therapy targeting unloading of muscle tension while the patient is waiting to schedule testing is not a poor clinical decision, but rather a prudent multidisciplinary approach to patient care for those who are anxious about not receiving prompt and proper treatment after many specialist visits.
In summary, MTDg is an often underdiagnosed condition that can lead to significant quality of life concerns for patients. MTDg has shown to be highly correlated with excessive laryngeal muscle tension and may exist with other concomitant laryngeal disorders, frequently those associated with irritable larynx syndrome. It is currently a diagnosis of exclusion and clinicians must be prudent in their evaluations to ensure no other causes exist. Studies have shown that therapy aimed at unloading laryngeal muscle tension has resulted in 100% of patients showing dysphagia symptom reduction [1], with an average symptom reduction of 90% [3]. It is important that this diagnosis be considered in the evaluation of dysphagia so a patient-centred treatment plan may be developed to help relieve patient suffering.
References
1. Kang CH, Hentz JG, Lott DG. Muscle tension dysphagia: symptomology and theoretical framework. Otolaryngol Head Neck Surg 2016;155(5):837-42.
2. Morrison M, Rammage L, Emami AJ. The irritable larynx syndrome. J Voice 1999;13(3):447-55.
3. Kang CH, Zhang N, Lott DG. Muscle tension dysphagia: contributing factors and treatment efficacy. Ann Otol Rhinol Laryngol 2021;130(7):674-81.
4. DePietro JD, Rubin S, Stein DJ, et al. Laryngeal manipulation for dysphagia with muscle tension dysphonia. Dysphagia 2018;33(4):468-73.