These authors from the speech and language therapy department at Imperial College Healthcare NHS Trust, describe their view of a patient-centred approach to managing dysphagia in complex laryngology. Careful consideration of the balance of airway, voice and swallow, which is personalised to the patient, is key.
Dysphagia, or difficulties eating, drinking and swallowing, is a difficult condition to manage in any clinical population, impacting on health and quality of life. The importance of this area of clinical practice is reflected by an ever-increasing body of literature. For clinicians working in the field of complex laryngology, this is especially true.
The larynx is key to breathing, swallowing and voice, and maintaining the delicate balance of these three functions is extremely challenging. In the majority of cases, the aim of surgical interventions is to improve the airway. However, this leads to disruption of swallowing and voice [1]. Within our airway practice, patients tell us, “I will always choose to breathe, but…”. The ellipsis is the space where speech and language therapists (SLTs) operate and represent the significant added value we can bring to complex laryngology multidisciplinary teams. SLTs manage swallowing and voice at every point in a patient’s journey in complex laryngology.
"The most important aspect of any assessment is talking to the person and establishing what their goals and priorities are in relation to swallowing, as well as voice and airway"
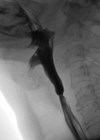
Swallowing disorders in complex laryngology can have several underlying aetiologies, including vagal nerve damage impacting sensory and motor functions in the pharynx and larynx (Figure 1), surgical intervention leading to oedema, sensitivity and airway compromise, post-radiotherapy changes, respiratory insufficiency and muscle tension. Patients often have coexisting diagnoses, such as neurological conditions, that complicate the clinical picture. A thorough, multidimensional assessment of a person’s swallowing is the first stage in maintaining the balance. At our centre, a thorough clinical swallowing evaluation includes a detailed case history, cranial nerve assessment, 100ml Water Swallow Test, and patient-reported outcome measures (PROMS) addressing voice and swallowing. Current oral intake and textures based on the IDDSI Framework are also recorded. An instrumental swallowing assessment should be undertaken to give a clear baseline of swallowing ahead of any surgical intervention. The decision about whether to complete a flexible endoscopic evaluation of swallowing (FEES) or videofluoroscopy (VF) depends on which aspect of swallowing is being evaluated. On occasion, both studies may be required and are complimentary.
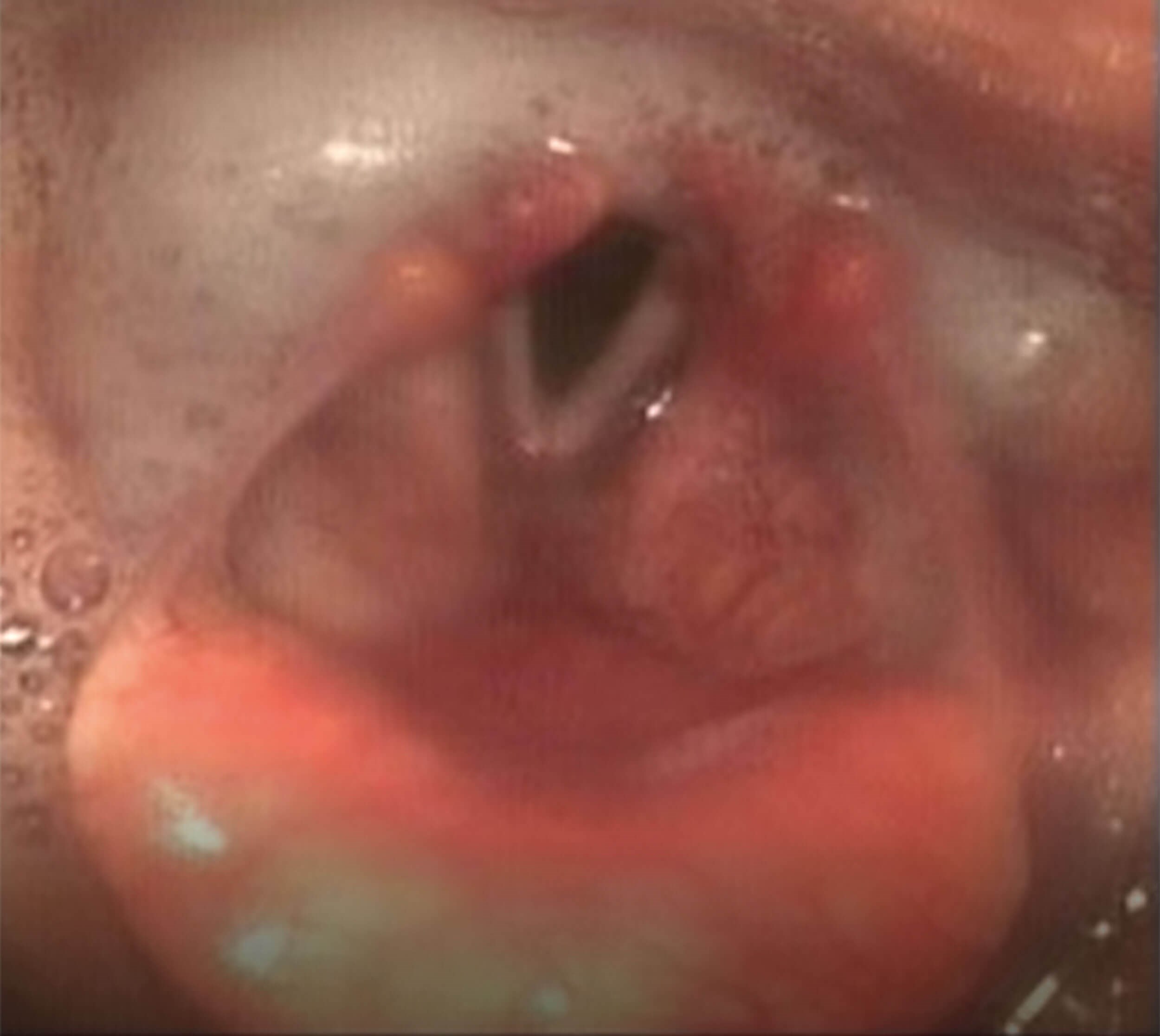
Figure 1. Image of pooled secretions entering posterior larynx via
interarytenoid space (absent sensation) and right vocal fold palsy,
with fully abducted left vocal fold in calm breathing.
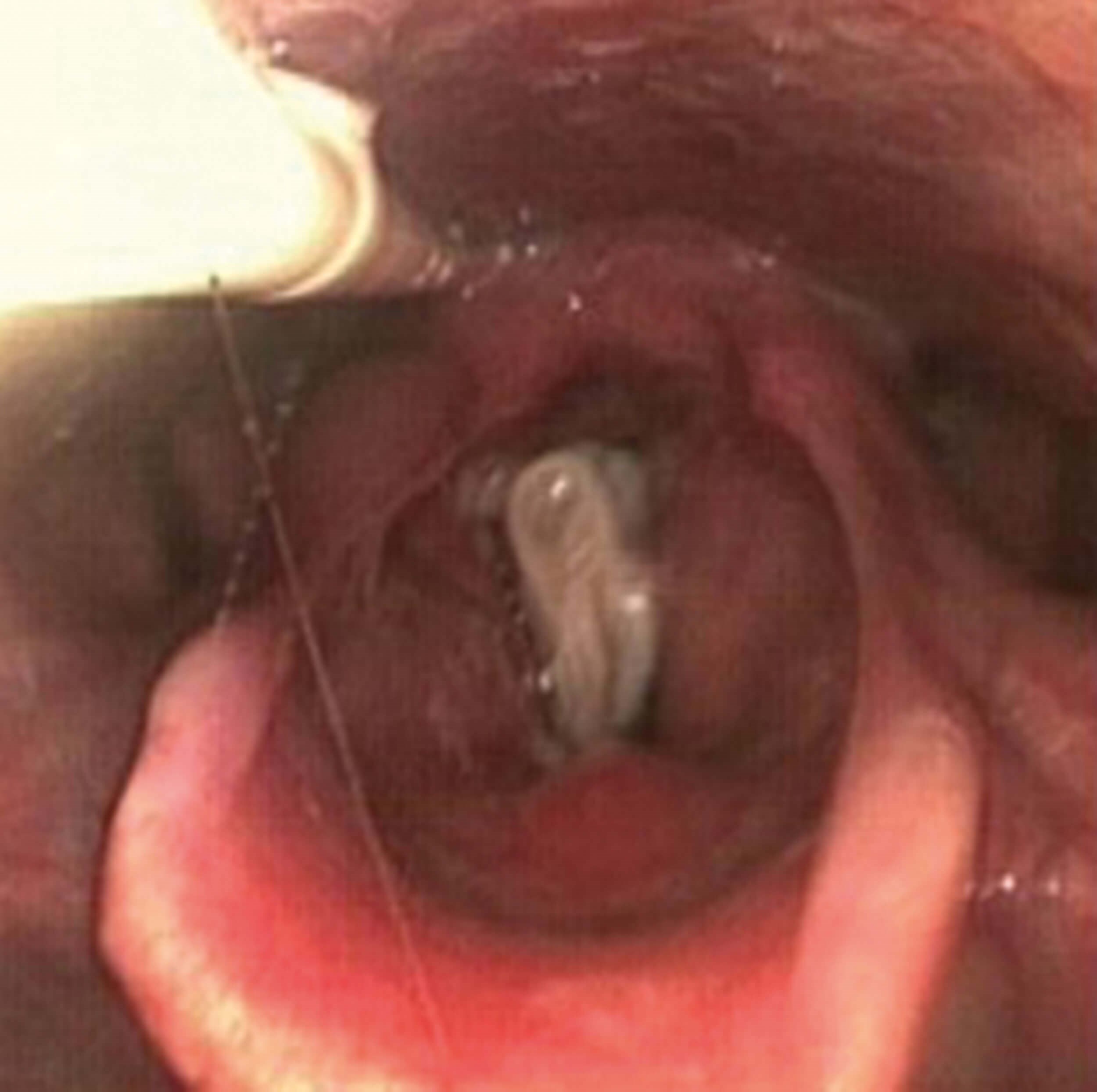
Figure 2. Image of larynx day one post laryngotracheal reconstruction with closed
stent and rib graft – stent visible between vocal folds within laryngeal vestibule.
However, the most important aspect of any assessment is talking to the person and establishing what their goals and priorities are in relation to swallowing, as well as voice and airway. Swallowing difficulties in the complex laryngology population can often be sub-clinical. This conversation can guide whether there are any subtle signs of challenge, for example always needing water at meals, taking a prolonged time with meals or being reluctant to eat out.
Some symptoms described by the complex laryngology caseload, such as globus, chronic cough and laryngeal hypersensitivity, overlap between being signs of swallowing and voice difficulty, hence the need for SLTs to be comfortable managing both presentations. This thorough, holistic assessment and the priorities of the person being assessed form the guide for management of their swallowing. Certain surgical procedures, such as arytenoidectomy or laryngotracheal reconstruction (Figure 2), are likely to disrupt swallowing in the short to medium term, and being clear with patients about what to expect in terms of recovery timeline is vital [1,2]. A clear understanding of the baseline function is necessary to ensure clinicians are not expecting a return to ‘normal’ swallowing, but to the criterion swallowing function of the individual.
"If we see an opportunity, rather than a problem, we can take uncertainty into our hearts and use it to drive and implement change and growth"
Management of swallowing difficulties is entirely individualised. For some patients, there may be a need to consider prehabilitation exercises in advance of surgery or other intervention in order to maximise their swallowing outcome, similar to the head and neck cancer population [1], although there are no studies as yet to determine the efficacy of this approach. Swallowing exercises can also be helpful post surgery to support rehabilitation of swallowing function. In all cases, instrumental assessment is key to selection of the most appropriate exercises. At our centre, therapeutic adjuncts such as expiratory muscle strength training (EMST) or inspiratory muscle strength training (IMST) have proved effective for certain individuals, particularly those with reduced cough strength and silent aspiration.

Figure 3. Image of supraglottic scar with vocal folds visible below.
One caveat that needs to be considered when implementing exercises for dysphagia, is the impact they may have on voice and, likewise, establishing which voice exercises may exacerbate dysphagia symptoms. A large proportion of the complex laryngology caseload have some degree of muscle tension dysphonia, and exercises focused on increasing effort in the pharynx or tongue base; for example, effortful swallow or Masako manoeuvre may have a negative impact on vocal function. Similarly, exercises which are typically used for deconstructing the laryngeal musculature to improve voice, such as yawn-sigh or twang, may reduce compensatory protective posture. Likewise improving expiratory airflow for cough and aspiration, on some occasions, can increase the intraglottal air pressure leading to a more forced collision of the vocal folds. Patient priority is key, and consideration of alternative exercises may be necessary.
Dietary modification is a useful tool for SLTs managing a dysphagia caseload. However, any decisions to alter the consistency of food and fluid a person is having can negatively impact quality of life (QOL) [3] and need to be considered carefully before implementation, alongside discussion with the person themselves. Where possible, we avoid completely nil by mouth decisions and allow free water from both a rehabilitative perspective as well as comfort and QOL. Clinicians must always consider that oral hygiene, tube feeding and dependence for feeding are far more likely to increase the risk of aspiration-related respiratory compromise than dysphagia [4].
Compensatory therapeutic techniques, such as a chin tuck to clear vallecular residue and increase airway protection, or a head turn to mitigate the impacts of a vocal fold palsy are helpful but are also best trialled under instrumental evaluation. A simple cough and clearing swallow technique or liquid wash through can often positively compensate for a person’s dysphagia.
Managing dysphagia in complex laryngology is challenging (Figure 3), but ultimately rewarding. Having a strong multidisciplinary and critically, person-centred approach is essential.
References
1. Clunie GM, Kinshuck AJ, Sandhu GS, Roe JWG. Voice and swallowing outcomes for adults undergoing reconstructive surgery for laryngotracheal stenosis. Curr Opin Otolaryngol Head Neck Surg 2017;25(3):195-9.
2. Rouhani MJ, Morley I, Lovell L, et al. Assessment of swallow function pre- and post-endoscopic CO2 laser medial arytenoidectomy: a case series. Clin Otolaryngol 2022;47(2):347-50.
3. O’Keeffe ST. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified? BMC Geriatr 2018;18(2):167.
4. Langmore SE, Terpenning MS, Schork A, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia 1998;13(2):69-81.