This article takes us through the diagnosis and management of swallowing problems common in older age. As our global population continues to grow and live longer, dysphagia will continue to be a global problem which needs to be recognised, understood and addressed.
The world is rapidly ageing. The global population over the age of 65 is expected to reach 1.5 billion by 2050. Swallowing complaints are extremely common among older adults and the evolving age demographic will have a tremendous impact on our healthcare system. The symptom of abnormal swallowing is known as dysphagia and the consequences of swallowing impairment include malnutrition, dehydration, social isolation, depression, aspiration pneumonia, lung abscess, and death.
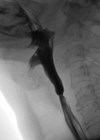
Dysphagia not only impacts the quality of life of those afflicted, but the disorder has profound implications on the social infrastructure and mental wellbeing of the affected individuals’ loved ones and caregivers. Many age-related illnesses are widely known to increase the risk of swallowing impairment (Table 1). It is essential for the otolaryngologist to have a thorough understanding of the challenges posed by the geriatric swallow and rapidly ageing population.
The process of swallowing is a reflexive action that most people perform over 1000 times daily. Swallowing safely and efficiently requires more than 25 muscle pairs across the oral cavity, pharynx, larynx, and oesophagus to function in a precise and coordinated fashion. Subtle but progressive anatomical and physiological changes occur with normal ageing that systematically diminish the functional capacity of the swallowing mechanism.
Swallowing challenges associated with ageing start in the mouth. Poor and absent dentition and ankylosis of the temporomandibluar joint can negatively impact deglutition. A larger, poorly masticated food bolus can challenge even a youthful, robust swallow. Atrophy and fatty infiltration of orofacial and lingual muscles is common and associated with aspiration in older adults. Laryngopharyngeal alterations attributed to age include diminished laryngopharyngeal sensitivity, prolonged swallow duration, delayed laryngeal vestibule closure, and diminished upper oesophageal sphincter opening. Healthy older adults may penetrate on up to 15% and may aspirate on up to 3% of swallows. As much of the body ‘sags’ with advancing age, so does the larynx.
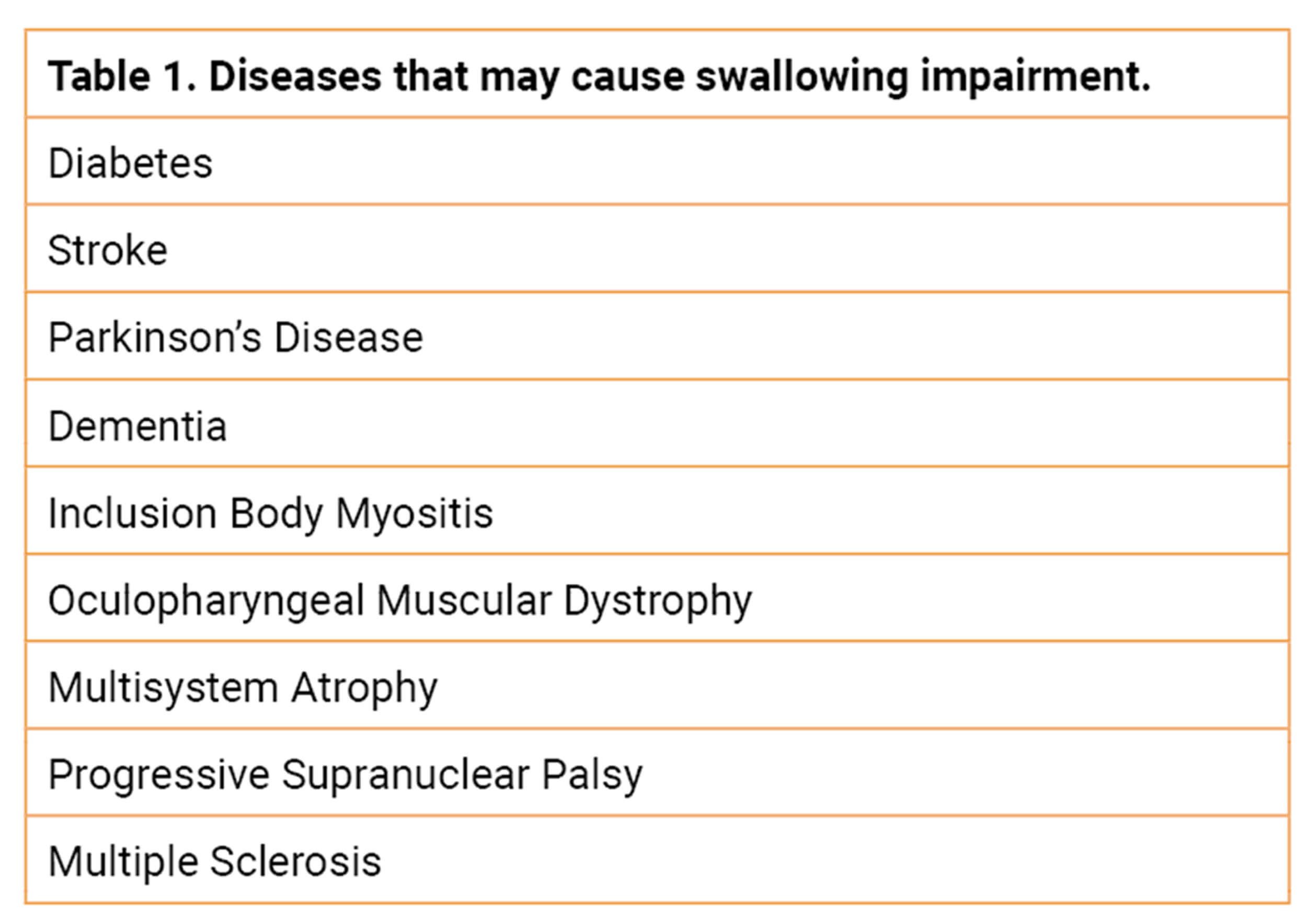
The lower position of the larynx in the neck negatively impacts opening of the upper oesophageal sphincter. Other factors that diminish upper oesophageal sphincter opening with advancing age include a 30% prevalence of cricopharyngeus muscle ‘bars’ in normal individuals >60 years of age and over a 60% prevalence of cricopharyngeal webs in elderly cadavers (Figure 1).
Figure 1. Cricopharyngeus muscle bar (a) and cricopharyngeal web (b).
The high prevalence of cricopharyngeal webs in the elderly is hypothesised to be secondary to the repeated mechanical trauma of the cricoid against the cervical spine that occurs over a lifetime of swallowing. The increased prevalence of cervical osteophytes with age contributes to this trauma and causes a further reduction in upper oesophageal sphincter opening. Although the hyoid bone attempts to compensate for this reduced opening with greater and prolonged elevation, these efforts fall short.
The larynx is also susceptible to age. The majority of persons over 65 years exhibit significant vocal fold atrophy. This can negatively impact both airway protection and pulmonary clearance. Although oropharyngeal and laryngeal impairments garner the majority of attention when it comes to investigating the effects of ageing on swallow, oesophageal dysfunction is equally as prevalent.
Although the prevalence of gastroesophageal reflux disease (GERD) approaches one quarter of the general population, nearly 30% of the elderly population receiving Medicare has received a prescription for an acid blocking medication. A lifetime of oesophageal inflammation from reflux contributes to oesophageal scarring, diminished peristalsis, delayed oesophageal emptying, and the symptom of dysphagia. The distal oesophagus is secured to the diaphragm via the phrenoesophageal ligaments. A person who lives to 80 will take nearly 700 million breaths in their lifetime. All of this breathing causes laxity of these ligaments, enlargement of the diaphragmatic hiatus, and predisposes older individuals to hiatal hernia (HH).
Lower oesophageal sphincter incompetence associated with HH is one of the primary factors responsible for the increased prevalence of GERD in the elderly. In fact, the prevalence of HH on CT imaging increases from only 2% in quadragenarians to 16% in septuagenarians. The incidence of adenocarcinoma of the oesophagus parallels the increased prevalence of GERD and HH in the elderly and peaks at 28/1000 males in the seventh decade of life. In addition to physiologic alterations in swallowing biomechanics that occur with ageing, various medications frequently used by the elderly not only become difficult to swallow but can actually contribute to dysphagia and swallowing impairment.
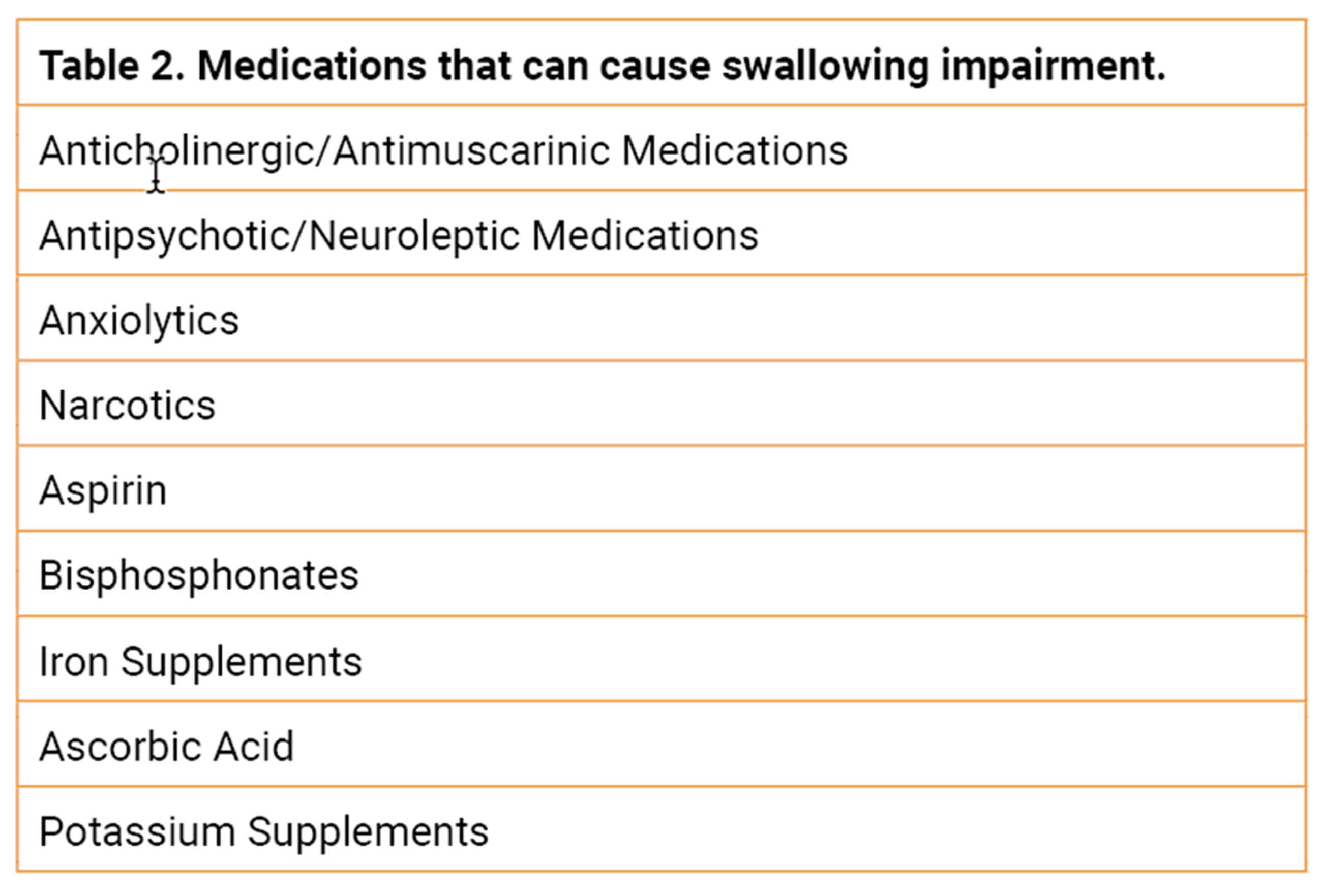
Up to 40% of Americans report difficulty swallowing pills. The most common sites of pill retention among the elderly in decreasing prevalence are the vallecula, upper oesophageal sphincter, the aortic arch, and the lower oesophageal sphincter. Alterations in orofacial and lingual muscle tone and diminished upper ooesophageal sphincter opening, as described previously, are the primary forces contributing to this difficulty. Calcification of the aorta, oesophageal stricture and neoplasm, and oesophagogastric outlet obstruction are secondary causes. The size, shape, and texture of pills and tablets all influence ease of consumption. In addition to the physical difficulty elderly people can experience swallowing pills and tablets, the systemic and caustic effects of certain medications and may cause dysphagia and swallowing impairment. Table 2 depicts the most common medications that can cause dysphagia in the elderly.
There is good news in regard to the swallowing challenges that are inevitable with healthy ageing. There are numerous diagnostic and therapeutic options currently available to identify and alleviate much of this difficulty. Primary care clinics may employ patient-reported outcome measures such as the Eating Assessment Tool (EAT10) and PILL5 to identify older individuals at risk. The modern swallowing clinic has access to advanced endoscopic equipment, swallowing fluoroscopy, high-resolution manometry, ambulatory pH testing, and impedance planimetry. Atrophy of the orofacial and lingual muscles is amenable to swallowing exercise. Dentures can help improve one’s ability to masticate a food bolus. Oral hygiene can help reduce the risk of lung infection. Disorders of upper oesophageal sphincter opening are easily treatable with simple dilation and endoscopic or open cricopharyngeus muscle myectomy when necessary. Glottal insufficiency resulting in diminished airway protection and cough can be treated by vocal fold medialisation. Acid reflux is readily treatable with dietary and lifestyle modification, antacids and alginates, antisecretory medication, and hiatal hernia repair and fundoplication in select cases. Swallowing therapy under the direction of a speech and language pathologist and respiratory muscle strength training are useful adjuncts.
Consultation with an appropriate dietician is essential to prevent malnutrition, sarcopenia, and frailty. Medication can frequently be formulated into liquid dosing, although great care should be given to crushing or otherwise modifying the formulation of pills and tablets that are meant to be delivered in long acting, sustained, extended, or otherwise modified release forms. In these cases, over-the-counter pill lubricants are readily available.
Dysphagia in older adults is common and has the potential to present significant detrimental effects on quality of life and successful ageing. While the ageing process remains inevitable, resulting changes to the swallowing mechanism do not necessarily establish unsafe or compromised function. Some degree of swallowing impairment, however, is part of the normal ageing process. It is imperative that the swallowing clinician understands these changes, assists the general practitioner in identifying individuals at risk, and has an advanced knowledge of all the currently available prevention and treatment strategies.
Further reading
1. Nations U. World Population Ageing 2017: Highlights. United Nations; 2018.
2. Verin E, Clavé P, Bonsignore MR, et al. Oropharyngeal dysphagia: When swallowing disorders meet respiratory diseases. Eur Respir J 2017;49(4):1602530.
3. Ortega O, Martín A, Clavé P. Diagnosis and management of oropharyngeal dysphagia among older persons, state of the art. J Am Med Dir Assoc 2017;18(7):576-82.
4. Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr Gerontol Int 2019;19(2):91-7.
5. Chen KC, Jeng Y, Wu WT, et al. Sarcopenic dysphagia: A narrative review from diagnosis to intervention. Nutrients 2021;13(11):4043.
6. Feng X, Todd T, Lintzenich CR, et al. Ageing-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol A Biol Sci Med Sci 2013;68(7):853-60.
7. Kim J, Hiura GT, Oelsner EC, et al. Hiatal hernia prevalence and natural history on non-contrast CT in the Multi-Ethnic Study of Atherosclerosis (MESA). BMJ Open Gastroenterol 2021;8(1):e000565.
8. Butler SG, Stuart A, Markley L, Rees C. Penetration and aspiration in healthy older adults as assessed during endoscopic evaluation of swallowing. Ann Otol Rhinol Laryngol 2009;118(3):190-8.