Patients suffering with problems with their voice, airway and/or swallowing can find their symptoms immensely distressing, and their care places a huge burden on healthcare systems. We hear from a world-leading laryngologist on current and future directions.
Field of interest
I always knew I wanted to be a surgeon; it suited my linear and problem-focused mind! There was a problem, and I would know how to fix it. Once I started medical training I was fascinated by the anatomy of the body and, in particular, the head and neck. This resulted in me undertaking training in otolaryngology. I felt this was such a crucial specialty, dealing with the unique things that make us human: speech, eating for pleasure and listening.
Laryngology was a natural fit – social occasions always revolve around food, drink and parlay and this was what I wanted to treat and how I saw myself helping my patients. After completing general ORL training in New Zealand, I was fortunate to develop my skills and undertake research at the University of California, Davis, working in the Speech and Swallow Centre with Dr Peter Belafsky. His passion for improving the management of swallow-impaired people was infectious and during my time there, I saw the vast need for better assessment, novel therapeutic approaches and meaningful ways to broaden our treatment paradigms in laryngology and bronchoesophagology.
Endoscopic equipment had radically improved during my formative training years, and the endoscopic approach made sense to me, being less invasive and transgressing fewer natural tissue boundaries than traditional open procedures. With the advent of improved optics and smaller calibre endoscopes, we had better access to, and views of, the aerodigestive tract than ever before. I found endoscopy fun, and the dual ability to achieve diagnostic and therapeutic goals appealed to my type A personality. The increasing scope of application of endoscopic techniques is inspiring. When one can perform laser therapy or a balloon dilation through an office-based endoscope and have the patient back home for afternoon tea with no anaesthetic hangovers, we are on the road to improved outcomes and reducing the burden of costs.
“Treating six patients in a morning under local anaesthesia compared to three patients under general anaesthesia for around one tenth of the cost is a game-changer”
Office-based treatment is a win-win scenario for both the health system and the consumer. It is faster, safer, equally accurate and, at times, can access areas that are not possible under general anaesthesia [1]. Treating six patients in a morning under local anaesthesia compared to three patients under general anaesthesia for around one tenth of the cost is a game-changer. It is incumbent upon us to equip our trainees with these skills for the future, so that they are facile and confident with endoscopic techniques and continue to expand the remit of office-based therapies.

Figure 1. Lateral image during fluoroscopic swallowing study, mid swallow, centred on the pharynx
demonstrating anterior vertebral lipping of C4 and C5 indenting the barium stream.
Current research
Our understanding of the biomechanics of deglutition influences our proposed therapy strategies. Surgical interventions for swallowing problems are limited and the need for novel treatments in this area, particularly related to the pharynx, is acute. Our clinical laboratory at the University of Auckland explores deglutitive physiology across the age spectrum from newborns to centurions. We have developed an objective and quantitative approach to analysing swallowing, incorporating videofluoroscopic (Figure 1), manometric and cough-reflex data. A picture of the individual’s physiologic impairment is produced and from this we design interventions, treatment plans and pathways for re-assessment.
Feedback allows us to refine or modify the process based on the response of the patient. Our lab has now published swallowing data for normal adults of all decades, the ageing swallow profile, a protocol for assessment of newborns, infants and children, data specific for neurological conditions, reflux disease, presence of secretions in the pharynx and how to quantify them, normal anatomic variations of the cervical spine and prevalence of asymptomatic upper oesophageal sphincter adaptations [2,3]. We are exploring normative paediatric swallowing measures, the spread effects of varied cross-motor interventions on speech and swallowing in neurological conditions, the influence of head and neck cancer therapy on pharyngeal manometric signatures and how exercise influences this, and pepsin as a diagnostic marker for pharyngeal disorders.
“This burgeoning area of research has strongly incorporated tissue engineering principles and molecular manipulation, with promising outcomes”
Sometimes new perspectives can drive innovation. Collaborations with our engineering school have led to the development of an oesophageal swallowing robot, which we have used to test oesophageal stent properties and pill characteristics related to pill transit [4]. We have also developed a voice regeneration algorithm, designed for use on a mobile device, for reconstructing disordered speech and even alaryngeal sound. Pushing the envelope surgically, we have implanted the University of California swallowing expansion device (SED) – a pin and plate implant sewn to the cricoid to enable the receiver to manually distract the UES to facilitate bolus transit (Figure 2).
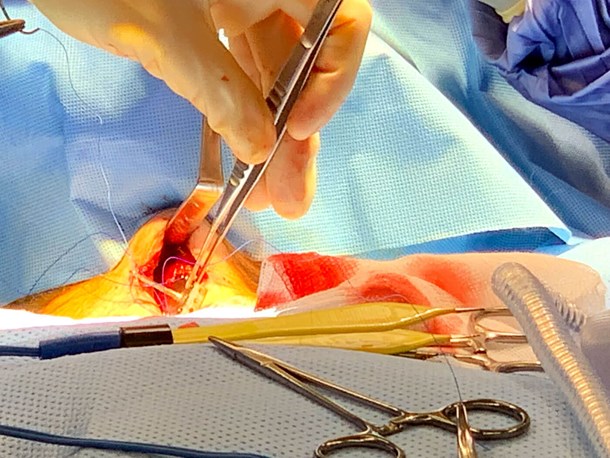
Figure 2. Photograph of the swallowing expansion device being held by
forceps and positioned for suturing into place onto the cricoid arch.

Figure 3. Photograph of excised ovine larynx demonstrating right vocal fold volume deficit post-biopsy.
Supraglottic tissue has been removed to assist stroboscopic assessment.
Note the relatively larger arytenoids of the ovine larynx as compared to human larynges.
In benchtop translational research, I have focused on the molecular basis for scar formation in the larynx and what pathways are most successful in moderating the wound healing response. This burgeoning area of research has strongly incorporated tissue engineering principles and molecular manipulation, with promising outcomes. We developed an ovine model of vocal fold injury (Figure 3) and examined the effect of currently utilised corticosteroid medications compared to a molecular signal inhibitor medication that ‘turns off’ production of collagen type 1A, or scar collagen [5]. There is exponential growth in the number of molecular targets now under exploration and an exciting degree of specificity in these treatments, that offers the potential to limit unwanted side effects seen with many traditional approaches.
“Molecular methods will be invaluable in future treatment paradigms including switching of signalling pathways, production of trophic factors and restitution of anatomical elements including 3D structures”
Visions for the future
The future is bright in laryngology. Many unsolved dilemmas remain to be vanquished. The sheer breadth of options to explore, and the uncharted territory that still exists, is stimulating. Pity there isn’t more time in the day! Molecular methods will be invaluable in future treatment paradigms including switching of signalling pathways, production of trophic factors and restitution of anatomical elements including 3D structures. Incorporation of 3D-printing techniques and new biomaterials will expand our ability to rebuild damaged architecture and preventative approaches will be incorporated during invasive therapies to mitigate downstream undesirable healing parameters. We must encourage our trainees to also undertake research and question the status-quo, and support them to continue evolving. It is important that we knowledge-share and collaborate – if COVID-19 has taught us one thing, it is that when we have a strong common goal, progress toward achieving it can be significant!
References
1. Amin MR, Postma GN, Setzen M, Koufman JA. Transnasal esophagoscopy: a position statement from the American Bronchoesophagological Association (ABEA). Otolaryngol Head Neck Surg 2008;138(4):411-14.
2. Dharmarathna I, Miles A, Fuller L, Allen J. (2020a). Quantitative video-fluoroscopic analysis of swallowing in infants. Int J Pediatr Otorhinolaryngol 2020;138:110315.
3. Dharmarathna I, Miles A, Allen J. Predicting penetration-aspiration through quantitative swallow measures of children: A videofluoroscopic study. Eur Arch Otorhinolaryngol 2021;278(6):1907-16.
4. Dirven S, Xu WL, Cheng LK, Allen J. Biomimetic Investigation of Intrabolus Pressure Signatures by a Peristaltic Swallowing Robot. IEEE Transactions on Instrumentation and Measurement 2015;64(4):967-74.
5. Allen J. Effect of corticosteroids vs halofuginone on vocal fold wound healing in an ovine model. Laryngoscope Investig Otolaryngol 2021;6(4):786-93.